Published: November 26, 2023 | 1 min read
How to Deal with Kidney Stones during Pregnancy
ARTICLE SHORTCUTS
- WHEN DO KIDNEY STONES FIRST APPEAR?
- POSSIBLE CAUSES OF KIDNEY STONES DURING PREGNANCY
- SYMPTOMS AND DIAGNOSTIC IMAGING
- TREATMENT OPTIONS
Bringing a new life into the world is not easy. Plus, if you have kidney stones, things will be more complicated. Sadly, roughly 1 out of every 200-1,500 pregnant women deal with kidney stones during their pregnancy.
And kidney stones can also trigger the following complications during your pregnancy:
- Gestational hypertension: high blood pressure without protein in the urine
- Preeclampsia: high blood pressure with protein in the urine
- Urinary tract infections: bacterial infection affecting the urinary tract
Fortunately, the rate of kidney stones during pregnancy is low. And we can even lower it by understanding the risk factors, symptoms, and how to diagnose/treat these stones.
WHEN DO KIDNEY STONES FIRST APPEAR?
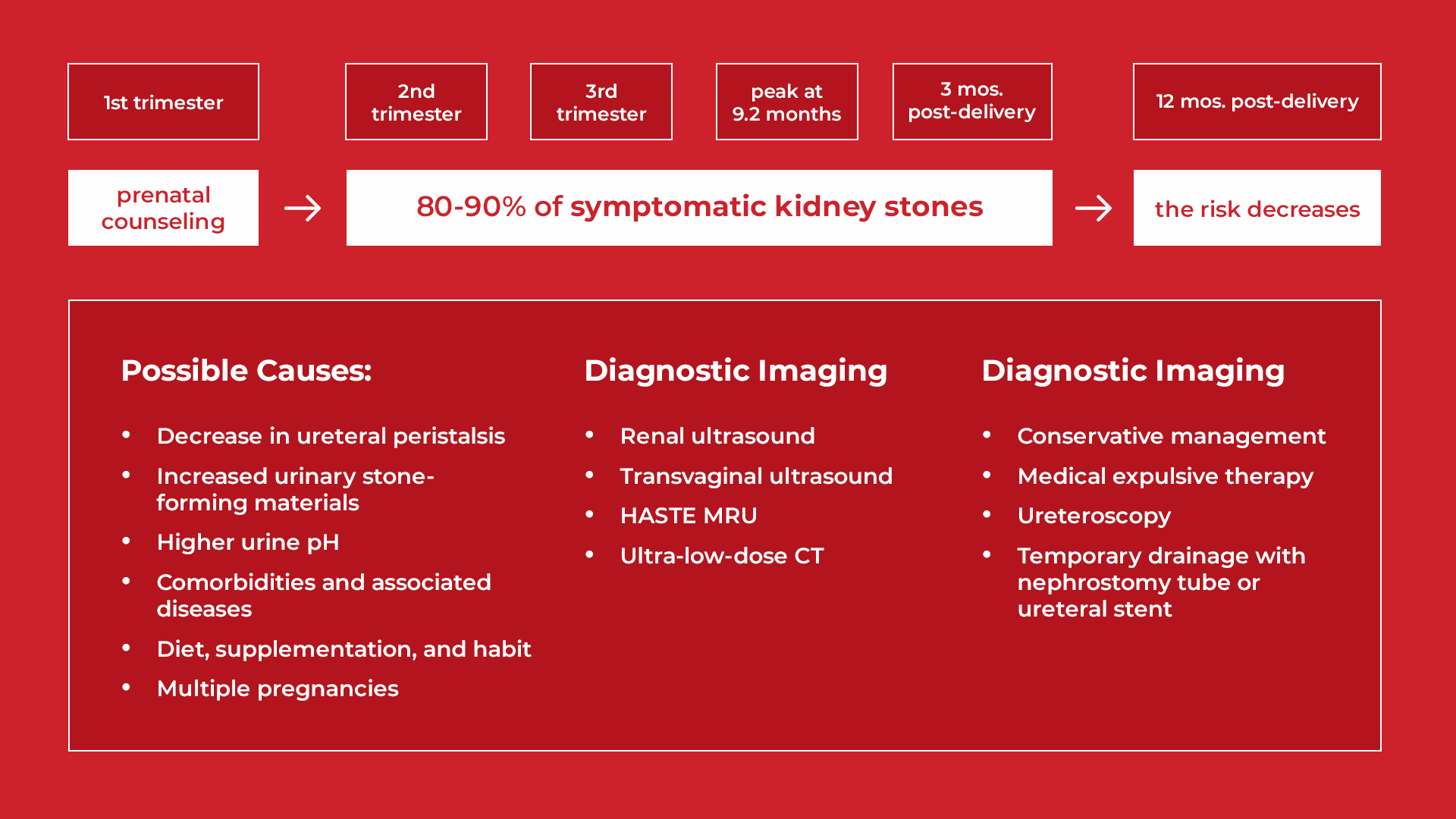
For most women, kidney stones may exist during the second (from week 15 through week 28) and third trimester (from week 29 through delivery). The peak is around the delivery time, up to 9.2 months after conception. Thus, the threat of kidney stones can continue until three months after delivery.
The risk of kidney stones remains high after delivery despite the changes in the body that lead to stones being resolved during pregnancy. Kidney stones take time to form and then enter the ureter, where they cause the initial pain. Fortunately, the odds of developing a kidney stone lower significantly 12 months after delivery. This is regardless of age, race, or history of obesity, diabetes, and hypertension. However, it is important to know that the chances of forming a kidney stone during pregnancy are higher in obese women (BMI > 30).
POSSIBLE CAUSES OF KIDNEY STONES DURING PREGNANCY
During pregnancy, hormonal changes can impact many risk factors for kidney stones. For example, an increase in the hormone progesterone leads to fewer ureteral peristalsis. Ureteral peristalsis is the series of constant contractions in the ureter that helps drive urine from the kidney to the bladder.
Also, as the uterus expands, it may compress some areas of the urinary tract leading to hydronephrosis. Hydronephrosis happens when urine gets trapped in the kidneys, draining slowly to the bladder. Luckily, it usually resolves within 4-6 weeks after giving birth.
Suppose urine cannot drain well (either from hydronephrosis or the reduction in peristalsis). In that case, it stays in the kidneys longer, which can lead to stone formation. Kidney stones form when elements such as calcium, oxalates, phosphate and uric acid have ample time and conditions to bind together in the urine. Sadly, the presence of sodium, calcium, and uric acid in the urine increases during pregnancy.
The placenta also produces more vitamin D to help the baby’s bone development. Additionally, many women are encouraged to take calcium and vitamin D supplements during pregnancy. These things can contribute to hypercalciuria in pregnancy. Hypercalciuria happens when excess calcium is in the urine.
Lastly, and most importantly, urine pH is also affected during pregnancy. The urine pH of pregnant women rises (becomes alkaline) because the hormone progesterone can alter the blood’s acid-base balance. Please note that alkaline urine may lead to calcium phosphate stones. That’s why the most common kidney stone type for pregnant women is calcium phosphate stones, which form richly in alkaline urine.
When urine becomes alkaline (pH >7.5), calcium may bind with phosphate instead of oxalate. Thus, the change in urinary pH explains why calcium phosphate stones (also known as (hydroxyapatite) are common in pregnant women.
Aside from pregnancy-related physical changes, the following conditions and habits can lead to kidney stones in pregnant women:
- Diabetes
- Hypertension
- Chronic Kidney Disease
- Gout
- Smoking
SYMPTOMS AND DIAGNOSTIC IMAGING
The most common symptom of kidney stones for pregnant women is flank pain (the agonizing pain below the rib and above the hip), according to 96.5% of 144 confirmed cases in one study. But, the typical signs and symptoms of kidney stones aren’t 100% reliable for pregnant women. Many new discomforts that pregnant women experience may also feel like kidney stones. Even blood in the urine, a common sign of a kidney stone, sometimes happens during pregnancy.
Because the fetus’ life is delicate, diagnostic methods become limited. For example, CT scans are the gold standard in identifying kidney stones. However, a CT scan is not an option for pregnant women due to radiation exposure concerns. The same is true for traditional X-ray imaging.
This leaves Ultrasounds and a few other imaging methods as options for pregnant women. However, ultrasounds are very weak at locating kidney stones. A study conducted among pregnant women admitted for kidney stones found that only 60% of stones were identified using ultrasound. If the diagnosis isn’t accurate, the pain and hydronephrosis from a stone may be mistaken as normal during pregnancy.
Below are a few options available to pregnant women for identifying kidney stones. Remember, though, this is not medical advice. Consult your medical team before making any decision that could impact your child.
Renal Ultrasound
Renal ultrasound is the most recommended imaging technique because it is not invasive. But as mentioned previously, it is pretty weak in identifying stones (34% sensitivity and 86% specificity). Even so, this method is totally safe for the child.
Transvaginal Ultrasound
Transvaginal ultrasound doesn’t use radiation too. Instead, it uses an ultrasound transducer in the vagina (unlike the traditional ultrasounds done outside the body). This technique is much better at identifying blockage in the lower (distal) urinary tract caused by a kidney stone or not.
Half-Fourier Single-Shot Turbo Spin Echo (HASTE) Magnetic Resonance Urography (MRU)
Another imaging method that your doctor may suggest is a HASTE MRU. The result is as accurate as a CT scan. However, unlike a CT scan that uses ionizing radiation, a HASTE MRU uses non-ionizing radiation. Here’s a brief description of these two types of radiation:
- Ionizing Radiation: strong enough to directly affect or damage atoms or DNA (ex: x-rays and gamma rays)
- Non-Ionizing Radiation: not strong enough to cause harm (ex: Wifi, AM/FM radio, and power lines)
Regarding safety, the 2013 ACR guidelines state that MRU imaging has no proven harmful effects on the fetus. Moreover, several studies of pregnancies with a history of MRU exposure in the first to third trimester found no evidence of increased danger to the developing child. However, using contrast agents such as gadolinium is dangerous and may cause newborn death.
TREATMENT OPTIONS
Options for managing kidney stones during pregnancy are limited too. Most modern techniques involve surgeries or medical drugs that may cause harm to the fetus. If you find yourself in this situation, it is best to develop a plan with your medical team that may include the following methods:
Conservative Management
Conservative management is anything that doesn’t involve surgery. Proper hydration is very important here. You can manage pain and pass your kidney stone if you get this right. Stone passage rates using conservative management are around 70-80%. However, this percentage may be overstated due to misdiagnosis and lack of follow-ups.
Additionally, you can add citrate (from citrus fruits) and magnesium to your water because they help reduce the formation of new stones. Please note that Nonsteroidal anti-inflammatory drugs (NSAIDs – like Advil and aspirin) are best avoided for the fetus’ safety. Tylenol can be used for mild pain. But, it may not be strong enough to deal with elevated pain levels.
Ureteroscopy
If conservative management fails, your doctor may recommend a Ureteroscopy. This procedure is done under either spinal or general anesthesia. It involves inserting surgical instruments through your urethra, into your bladder, and then into the ureter or kidney. How far up they go into the urinary tract depends on the stone’s location.
A ureteroscope (surgical camera) is used to clearly locate the stones. Commonly, this procedure requires X-ray guidance. However, strategies to reduce radiation exposure are now practiced to keep the fetus safe. These include using low-dosed and pulsed fluoroscopy (X-ray) and lead-shielding of the patient’s pelvis.
But if you want zero radiation, it’s possible. One way to do it is by visualizing the passage of the ureteroscope using a tiny camera inside. Ultrasound-guided ureteroscopy is also another way.
Temporary Drainage
Temporary drainage involves the use of a ureteral stent or a nephrostomy tube. While this method is invasive, it is quick, performed with minimal anesthesia, and does not need radiation exposure.
- Ureteral Stent: a small plastic tube placed inside the ureters through the urethra. This helps urine pass from the kidney to the bladder.
- Nephrostomy Tube: a thin plastic tube is inserted from the back (through the skin into the kidney) to collect urine. The urine then goes to the collection bag worn outside the body.
Note that both of these are short-term solutions to drain urine that was trapped due to blockage. Since draining urine lowers pressure on the kidney, the pain is relieved.
If you’re looking for more in-depth guidance on how to manage kidney stones during pregnancy, check out our Coaching Program to get access to the information and support you need.
References
- Risk of Symptomatic Kidney Stones During and After Pregnancy
- Contemporary best practice urolithiasis in pregnancy
- Management of urolithiasis in pregnancy
Comments or questions?
Responses
You must be logged in to post a comment.

order sildenafil online uk
order sildenafil online uk
cialis not working first time
cialis not working first time
generic viagra quick delivery
generic viagra quick delivery
tadalafil 20mg canada
tadalafil 20mg canada
buy cialis canadian
buy cialis canadian
viagra pills online in india
viagra pills online in india
cialis online mastercard
cialis online mastercard
cost of vicodin pharmacy
cost of vicodin pharmacy
percocet price pharmacy
How to Deal with Kidney Stones during Pregnancy | Stone Relief
domperidone inhouse pharmacy
How to Deal with Kidney Stones during Pregnancy | Stone Relief
first rx pharmacy statesville nc
How to Deal with Kidney Stones during Pregnancy | Stone Relief
buy vyvanse online pharmacy
How to Deal with Kidney Stones during Pregnancy | Stone Relief
history essay help
How to Deal with Kidney Stones during Pregnancy | Stone Relief
college application essay writing service
How to Deal with Kidney Stones during Pregnancy | Stone Relief
help write essay online
How to Deal with Kidney Stones during Pregnancy | Stone Relief
essaywriting service
How to Deal with Kidney Stones during Pregnancy | Stone Relief
help with writing essay
How to Deal with Kidney Stones during Pregnancy | Stone Relief
college essay help nyc
How to Deal with Kidney Stones during Pregnancy | Stone Relief
custom essays essay help
How to Deal with Kidney Stones during Pregnancy | Stone Relief
Proper hydration really goes a long, long way in both the prevention and treatment of kidney stones ????