Published: March 20, 2022 | 43 mins read
Percutaneous Nephrolithotomy (PCNL) for Kidney Stones
Article Shortcuts
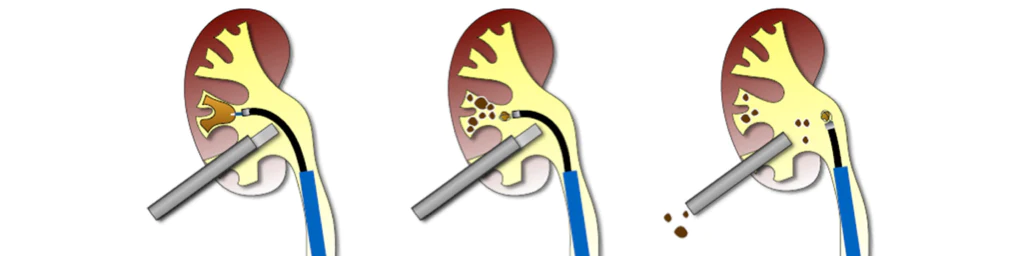
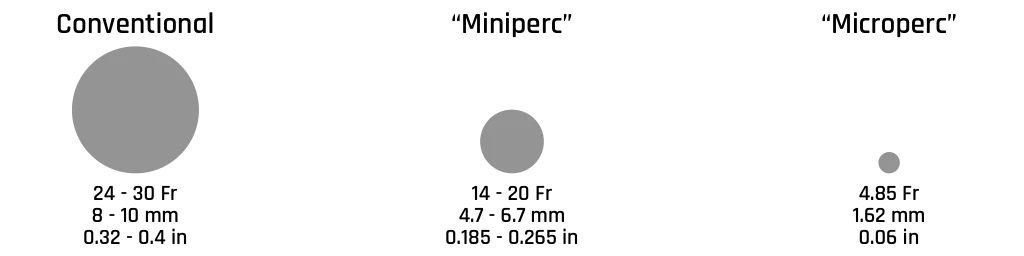
Percutaneous Nephrolithotomy (PCNL) was first described in 1976 as an operative technique for removing kidney stones through a percutaneous nephrostomy tract that involves an incision into the skin and kidney. Since its introduction, there have been many technological improvements (such as Miniperc and Microperc) over the last few decades that have led to Percutaneous nephrolithotomy (PCNL) becoming one of the cornerstone treatments for large (> 2cm) or staghorn kidney stones.
- Percutaneous: made, done, or affected through the skin
- Nephro: of a kidney; relating to the kidneys
- Lithotomy: surgical removal of a stone from the bladder, kidney, or urinary tract

AMERICAN UROLOGICAL ASSOCIATION PATIENT SELECTION CRITERIA
In the treatment of adult patients with ureteral stones:
- In patients who fail or are unlikely to have successful results with Shockwave Lithotripsy (SWL) and/or Ureteroscopy (URS), clinicians may offer Percutaneous Nephrolithotomy (PCNL), laparoscopic, open, or robotic-assisted stone removal.
In the treatment of adult patients with renal stones (stones still in the kidney):
- In symptomatic patients with a total renal stone burden > 20 mm, clinicians should offer Percutaneous Nephrolithotomy (PCNL) as first-line therapy.
- In patients with symptomatic calyceal diverticular stones, endoscopic therapy (URS, PCNL, laparoscopic, robotic) should be preferentially utilized.
DIAGNOSIS

Imaging
Several imaging techniques have been described to diagnose kidney stones in our Kidney Stone Imaging blog. Ultrasound (US), computerized tomography (CT), and plain X-rays are most commonly used.
Non-contrast CT has emerged as the imaging technique of choice because of its relative cost-effectiveness, sensitivity for identifying stones, and speed at which it can be performed. In non-obese individuals (BMI less than 30), low-dose CT is an acceptable option for reduced radiation exposure.
In cases of a significant stone burden, computerized tomography (CT) aids in the classification of stone size, location within the collecting system, and stone density. Additionally, CT scans assist Surgeons with determining the operative approach they may take to gain access to the stone.
In regions of the world where computerized tomography (CT) is not readily available, Ultrasound (US) is a reasonable alternative. Unfortunately, though, sensitivity and specificity are not as high as CT (see below for a comparison).
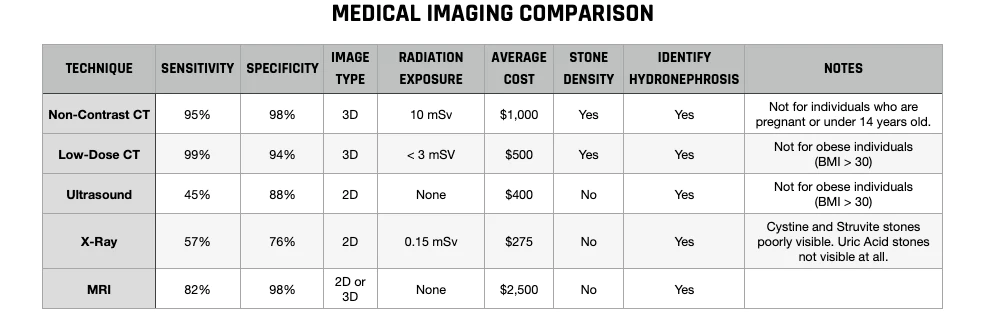
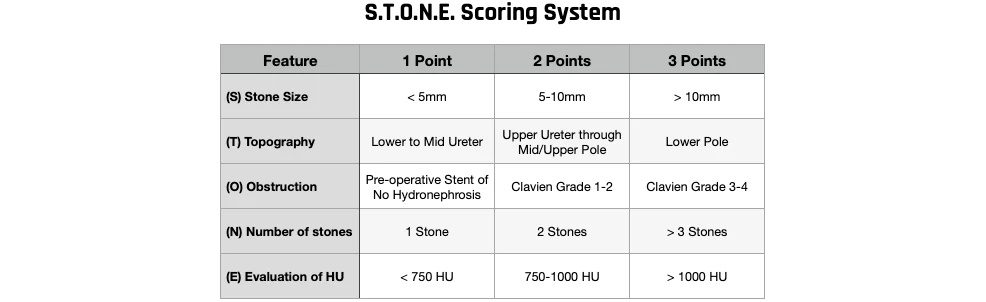
STONE Scoring System
In 2014, Okhunov et al. proposed the STONE scoring system to standardize Percutaneous Nephrolithotomy (PCNL) reporting. The STONE scoring system measures five variables relating to stone complexity based on pre-operative CT scan scored on a 1-3 point scale for each component:
- (S) Stone size
- (T) Topography (location of stone)
- (O) Obstruction
- (N) Number of stones present
- (E) Evaluation of HU (stone density)
Okhunov found that the pre-operative STONE score correlated to post-operative stone-free rate, estimated blood loss, operative time, and length of stay. In a follow-up multi-institutional study, results confirmed that a higher STONE score correlated with lower stone-free rates, increased bleeding and estimated blood loss, operative time, length of hospital stay, fluoroscopy time, and overall complication rate.
PRE-OPERATIVE PLANNING
Anticoagulation & Anti-platelet Therapy
The number of individuals requiring Percutaneous Nephrolithotomy (PCNL) on long-term anticoagulation or anti-platelet therapy has increased in recent years due to the use of more drug-eluting cardiac stents, heart valve replacements, treatment of atrial fibrillation, and cardio-protective measures. However, controversy exists as to which patients may safely be taken off anticoagulation for a period of time and how to manage patients who need to remain on anticoagulation during the operation.
In patients that cannot stop anticoagulation that have a significant stone burden, staged Ureteroscopy (URS) may be preferable to Percutaneous Nephrolithotomy (PCNL). In patients with significant cardiac risk factors, stopping aspirin may have adverse cardiac consequences during the procedure. Fortunately, recent studies have shown that low-dose aspirin can be safely continued during the procedure without a significant risk of bleeding.
In patients undergoing procedures with a high risk of bleeding, such as Percutaneous Nephrolithotomy (PCNL), it is recommended that they discontinue the use of warfarin 3-5 days before the procedure. Based on the results of a study conducted by Kefer et al., the study recommends stopping warfarin 5 days before surgery and waiting another 5 days to restart. Low molecular weight heparin may be used to bridge the time that warfarin is stopped and restarted.

Body Mass Index (BMI)
Shockwave Lithotripsy (SWL) is the first-line treatment preference for stones in the kidney less than 2cm. However, the application of SWL in obese individuals (BMI> 30) is a challenge due to the increased distance between the stone and the skin. Difficulty is also seen regarding fluoroscopic/ultrasonic imaging and the weight-bearing capacity of the SWL equipment. Therefore, Ureteroscopy (URS) has been suggested as an alternative for obese individuals. However, in individuals with a more significant stone burden, longer operative times prevent the widespread use of URS.
In current times, Percutaneous Nephrolithotomy (PCNL) is the most frequently used treatment in obese and morbidly obese individuals with stones in the kidney. However, Urologists are confronted with many problems during the procedure due to the overweight nature of the individual. For example, positioning the patient on the operating table will require the help of several health care personnel. Additionally, pressure points along the body should also be supported with pads to avoid the formation of pressure sores.
Supporting the patient is especially important while performing Percutaneous Nephrolithotomy (PCNL) in the prone position with obese individuals. Due to their weight, significant compressive forces are being applied to their chest and lungs, leading to respiratory issues in individuals with restricted lung capacity. In addition, compression of the vena cava inferior decreases blood flow return, potentially triggering cardiac complications. Some opinions favor the supine (face up) position for obese individuals. The supine position may reduce cardiac and respiratory problems. However, this has not been thoroughly studied or validated.
Vena Cava Inferior: large blood vessel responsible for transporting deoxygenated blood from the lower extremities and abdomen back to the right atrium of the heart)
Increased BMI complicates Percutaneous Nephrolithotomy (PCNL) procedures concerning both anesthetic risks and technical maneuvers during surgery. Due to the above-average thickness of the body fat in obese individuals, the length of the nephroscope or Amplatz sheath may not permit access into the renal collecting system or make contact with the stone. A study performed by Curtis et al. described a method for incising and retracting the skin and body fat to gain extra distance. However, this is very invasive and is not commonly used.
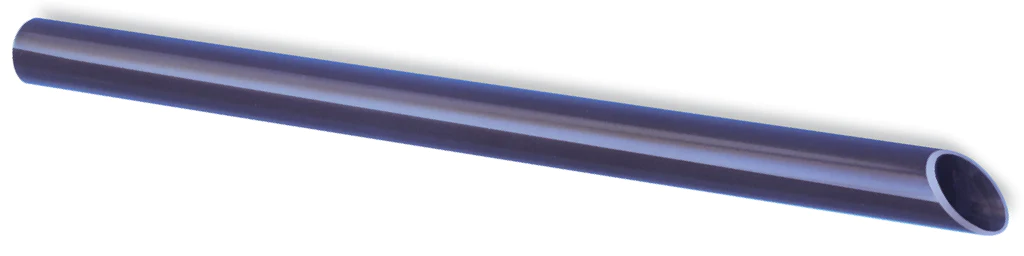
Amplatz Sheath: a hollow device designed to allow smooth passage of surgical instruments into the nephrostomy tract
Another study recommended using a nephrostomy tube inserted a week before the Percutaneous Nephrolithotomy (PCNL) procedure. This method allows the nephrostomy tube to create an access tract between the skin and kidney.
Despite the unfavorable effects of obesity on Percutaneous Nephrolithotomy (PCNL) procedures, many current studies have revealed this procedure’s success and safety. For example, a study conducted by Carson et al. found that there was no difference between obese and non-obese individuals in terms of operative times, stone-free rates, and complication rates. Another study performed by Pearle et al. investigated Percutaneous Nephrolithotomy (PCNL) procedures with multiple groups of obese individuals and found that while operative time was longer, the stone-free rate and complication rate were comparable.
As a concluding remark, Percutaneous Nephrolithotomy (PCNL) is a safe, effective, and reliable treatment method for stones in the kidney less than 20mm in obese patients.
Stents
The use of a pre-operative stent can aid access. However, pre-operative stent use has been found to significantly increase the odds of a patient meeting ≥ 2 SIRS criteria post-operatively. This has been further confirmed by estimating urosepsis using q-SOFA, which showed a 27% increase in the odds of getting urosepsis when a pre-operative stent was used.
NOTE: SIRS (Systemic Inflammatory Response Syndrome) and q-SOFA (Quick- Sepsis-Related Organ Failure Assessment) are criteria-based systems to help medical professionals determine the risk for sepsis after a surgical procedure. More details on this subject can be found in the Complications section below.
At the time of this writing, no known studies have linked pre-operative Percutaneous Nephrolithotomy (PCNL) stent use to urosepsis. However, a prior study by Mikes et al. found that pre-operatively stented patients were at greater risk for serious infection-related complications following Ureteroscopy (URS). This is possibly due to bacterial colonization and biofilm formation. When these “colonized’ stents are moved around during the procedure, bacteria can spread; thereby increasing the risk of urosepsis.
NOTE: Ureteral stents may also predispose patients to urosepsis. Stents are thought to facilitate retrograde (against the urine flow) bacterial ascent from the bladder to the kidneys by serving as a conduit.
An in vitro study (test-tube study) conducted by Hobbs et al. demonstrated the ability of Proteus mirabilis (a urea-splitting bacteria) to move from the bladder to the kidneys by forming biofilm communities along the length of the ureter. Ureteral stents may enhance this process as conditioning films readily form on stent surfaces and provide the necessary surface for bacterial adhesion. Together, these mechanisms can contribute to the systemic spread of bacteria initially localized in the urinary tract.
Antibiotic Exposure
Antibiotic use before Percutaneous Nephrolithotomy (PCNL) remains a controversial topic. Using antibiotics before PCNL previously demonstrated a reduction of post-operative sepsis in individuals with negative pre-operative urine cultures. However, a recent study by the EDGE (Endourology Disease Group for Excellence) consortium demonstrated that pre-operative antibiotics do not reduce post-operative infections after PCNL.
This finding is further supported by a study conducted by Potretzke et al., who found extended antibiotic use during surgery did not reduce the risk of Systemic Inflammatory Response Syndrome (SIRS) after Percutaneous Nephrolithotomy (PCNL). Antibiotic exposure has been suggested to place pressure on the unitary microbiome for multi-drug resistant (MDR) bacteria. The mere presence of MDR pathogens serves as a risk factor for infection post-PCNL.
Lastly, Taisan et al. showed that exposure to oral antibiotics within 3-6 months might contribute to stone disease by altering the urinary microbiome to facilitate stone growth. Thus, pre-operative antibiotic use may work against you in terms of overall stone size. Additionally, in some cases, it may worsen the infection.

Struvite “Infection” Stones
Struvite stones account for roughly 10% of all kidney stones. These stones are produced in the presence of urea-splitting bacteria. These bacteria are associated with urinary tract infections with urease-producing bacteria that split urea to ammonium and increase urine pH to neutral or alkaline values. Organisms splitting urea are Proteus, Pseudomonas, Klebsiella, Staphylococcus, and Mycoplasma.
Due to their association with bacteria, several infection-related complications can arise following kidney stone treatment. One such complication is urosepsis. Fortunately, rates of urosepsis following the treatment of kidney stones are low (0.3-4.7%). However, while urosepsis is an uncommon complication following kidney stone treatments, it is a life-threatening complication that struvite patients are at an increased risk of developing.
Patients with struvite stones have been documented to be at an increased risk for experiencing infection-related complications post-operatively. However, within the population of struvite patients, factors that may predispose some to urosepsis have yet to be made clear. Understanding these factors can play a crucial role in optimizing patient care.
When SIRS and q-SOFA approximated urosepsis, univariable analysis (single variable) demonstrated that longer operative times and greater stone size were risk factors for urosepsis. While not specific to struvite stones, longer Percutaneous Nephrolithotomy (PCNL) operative times and larger stone size have been identified as risk factors for SIRS or post-PCNL sepsis.
SIRS: Systemic Inflammatory Response Syndrome
q-SOFA: Quick- Sepsis-Related Organ Failure Assessment
Bigger stones sizes may lead to longer operative times due to the increased complexity of treating larger stones. In addition, other factors such as the difficulty of access, renal bleeding, and patient physiology may also result in longer procedure times. Given the findings of many studies, considerations should be taken to stage Percutaneous Nephrolithotomy (PCNL) procedures for larger stones to minimize operative time and reduce the risks of urosepsis.
Higher pre-operative white blood cell (WBC) counts are an independent risk factor for a positive SIRS classification post- Percutaneous Nephrolithotomy (PCNL) for struvite stones. SIRS-positive patients had a significantly greater mean pre-operative white blood cell count. Although the white blood cell counts do not reflect true leukocytosis (elevated white blood cell counts), individuals with elevated but normal white blood cell counts may be at higher risk for progressing to urosepsis post-operatively. This indicates a state of increased systemic inflammation and/or subclinical disease. During PCNL, surgical trauma can induce further inflammation and enhance bacterial dissemination into the circulation. This can then lead to fulfilling SIRS criteria and, in turn, urosepsis.

Anesthesia
Most Urologists prefer general anesthesia for Percutaneous Nephrolithotomy (PCNL). This preference is due to the high level of anesthesia achieved, the ability to control the patient’s breathing, and because it is more comfortable for the patient. However, general anesthesia is more likely to cause drug-induced anaphylaxis, complications with endotracheal tube insertion, and cardiovascular, pulmonary, and neurological complications.
Regional anesthesia permits fine muscle relaxation and chives excellent surgical outcomes. Furthermore, regional anesthesia has been reported to reduce the risk of bleeding during surgery, less post-operative pain, and faster recovery times. Additionally, regional anesthesia is 40% less than general anesthesia in terms of cost.
In the end, the outcomes of Percutaneous Nephrolithotomy (PCNL) conducted using either general or regional anesthesia are similar. Nevertheless, regional anesthesia requires fewer hospital stay days and is associated with lower post-operative fever rates.

Hospital Stay Duration
The mean hospital stay is 2.9 days. All patients are admitted one day before surgery and stayed for 1-2 days after the procedure.
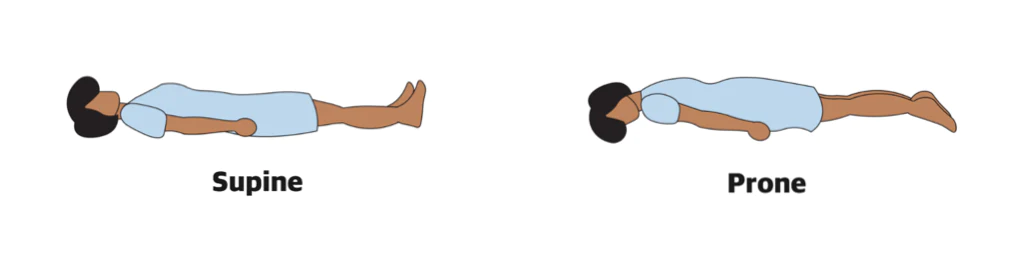
PATIENT POSITION
There are currently no guidelines for the use of supine (face-up) or prone (face-down) position on patients in Percutaneous Nephrolithotomy (PCNL). In supine PCNL, the nephroscope is inserted from below through a horizontal or slightly downward inclined Amplatz sheath. This angle uses gravity to drain the irrigation fluid and the stone fragments. Accordingly, the kidney’s collecting system is less distended, and the internal pressure may be lower in the prone position, which may cause reduced vision and working space. But potentially reduces the risk of post-operative infection.
Despite the possibility of lower intrarenal pressure in supine Percutaneous Nephrolithotomy (PCNL), fragments can descend into the ureter more easily than in the prone position due to gravitational effects. However, this is not a problem in endoscopic combined intrarenal surgery (ECIRS) because a flexible ureteroscope is positioned in the ureter. This is both to occupy that position and detect fragments that might drain into the ureter.
In a meta-analysis of 15 randomized controlled trials with a total of 1,474 patients, lie et al. reported supine versus prone position in Percutaneous Nephrolithotomy (PCNL) and found that operative time in the supine position was shorter. Furthermore, these investigators found lower rates of post-operative fever in the supine position than in the prone position.
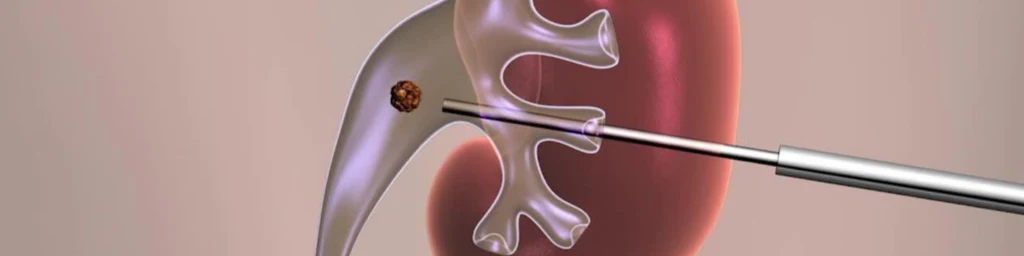
ACCESS
The successful establishment of the percutaneous renal channel is the basis for Percutaneous Nephrolithotomy (PCNL). Accurate puncture and dilation (widening) of the target kidney calyces (see below) are the keys to establishing the percutaneous renal cannel. However, the renal cortex (shown below) is relatively thick, and the space between the target calyces is limited.
Due to these factors, routine Percutaneous Nephrolithotomy (PCNL) puncture and dilation are associated with bleeding and channel loss risks. Therefore, the selection of the best PCNL approach forms still a challenge for urologists.

Inferior Vs. Superior Calyces Access
Traditionally, access from the back into the lower kidney is considered the safest percutaneous access to the internal collecting system of the kidney. This approach is widely practiced for access to stones in the renal pelvis, lower calyx of the kidney, and staghorn stones. However, this may not be an ideal access point for stone removal in all circumstances. Superior calyceal access is often underutilized due to fear of an intercostal puncture, risk of possible bleeding, and thoracic complications.
Intercostal Puncture: puncturing the intervening lung, pleura, liver, and spleen with the needle.
To investigate this further, we will look to a 2020 study by Amaresh et al. that compared the safety of superior calyceal access and inferior calyceal access. This study evaluated 126 patients between July 2018 and February 2019. Patients were split into two groups, Group I subject to superior calyceal access and Group II inferior calyceal access.
As we will see shortly, this study confirms that superior pole access has significant benefits over inferior pole access in patients with renal pelvis stones and/or lower pole kidney stones. Patients in Group I (superior calyceal access) enjoyed higher stone-free rates and fewer complications.
The choice of access is crucial and has resulted in a vigorous debate. Traditionally, the choice has been limited to superior or inferior calyceal access. However, with the introduction of Miniaturized Percutaneous Nephrolithotomy (Miniperc), middle pole access to the kidney has gained popularity.
Superior calyceal access provides certain technical and anatomical advantages. The upper pole directed posteriorly makes it closer to the posterior flank wall in the prone position. This provides for the shortest access tract. From an anatomical perspective, the upper calyx is usually drained by a single calyceal infundibulum (a funnel-shaped cavity or structure) in most people.
As seen in the photo above, the superior calyx also gives straight-line access to all calyces and Ureteropelvic Junction (UPJ) at minimum angulation. This straight-line access provides excellent visualization of the superior calyx, pelvis, ureter, and anterior/posterior inferior calyces.
The ease of operability increases with superior calyceal access, as demonstrated in the data for less operative time and fewer complications. This can be attributed to the guidewire comfortably entering the pelvicalyceal system during the initial puncture.
In the inferior calyceal access for stones in the renal pelvis or impacted stones in the lower calyx, slippage, bending, and kinking of the guidewire is seen when passed through the percutaneous puncture needle and often makes tract dilation difficult. This leads to guidewire migration, bending, slippage, and under-dilation of the tract.
In this study, 6.34% of patients in the inferior calyceal group required a repeat puncture due to guidewire dislodgment and displacement. This technical difficulty may be responsible for more bleeding and increased iterative times.
Superior calyceal access allows for easy manipulation of the nephroscope into distal (lower) calyces and upper ureter with minimal torque on the parenchyma. This provides for minor bleeding and facilitates the removal of fragments migrating during fragmentation to other calyces and/or upper ureter. Intrarenal navigation through the lower pole calyces is associated with angulation and torque on the pelvicalyceal system, often leading to unnecessary trauma and bleeding that may be avoided by superior calyceal access.
Parenchyma: The solid part of the kidney where waste excretion takes place.
Cortex: The outer layer of the parenchyma consisting of connective tissue.
Of note, when it comes to this study, patients in Group I (superior calyceal access) had larger sized access compared to Group II (inferior calyceal access). Since the superior calyx is a compound calyx, most Surgeons will select larger tract dilation. This allows for an easier puncture, comfortable dilation, and fast stone clearance. This study’s shorter operative time is related to the larger-sized access used in 80.9% of patients in both groups. Sheath sizes used range from 28-32Fr.
Compound Calyx: multiple papillae empty into a single calyx and infundibulum. They are more common in the upper pole of the kidney.
The ease of calyceal access and dilation made the stone clearance a straightforward exercise. As a result, the complete stone clearance rate was significantly higher in the superior calyceal access group at 96.82% when compared to the inferior calyceal access group at 85.71%. In addition, stone-free rates from isolated renal pelvis and lower calyceal stones were significantly higher in the superior calyceal group than the inferior calyceal group.
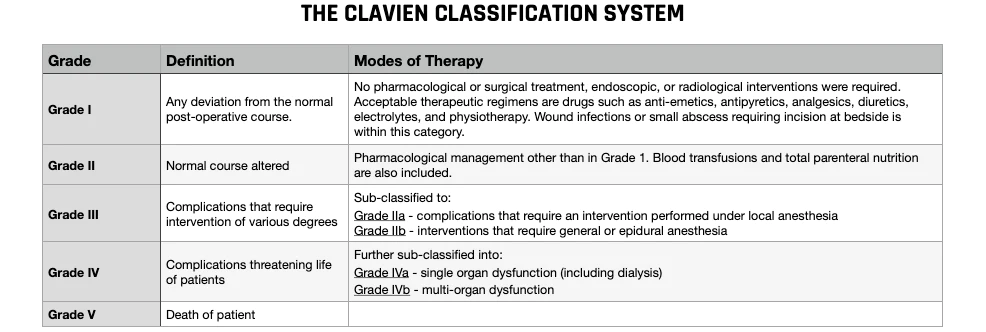
Although not statistically significant, the overall complication rate as classified by the modern Clavien grading system (see image above) was higher in the inferior calyceal access group (17.4%) compared to the superior calyceal access group (11.1%). A smilier trend has been observed in several other studies. Additionally, residual stones demanding a second-look procedure were reportedly higher in the inferior calyceal access group, which was statistically significant (2% vs. 18%).
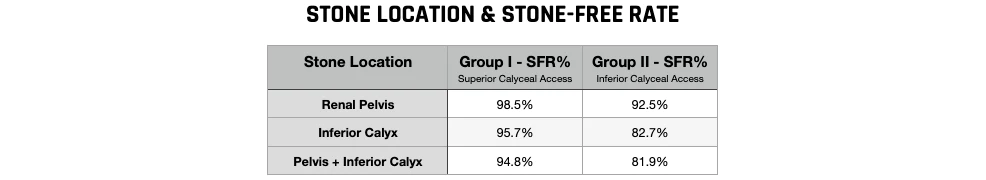
In conclusion, on this topic, superior calyceal access offers ease of access, dilation, and intrarenal navigation into most of the calyces. Furthermore, superior calyceal access is better than inferior calyceal access. This is primarily because one can achieve a complete and faster stone clearance with fewer punctures, shorter operative time, minimal risk of complications, and less need for additional procedures with minimal incidence of injury to the calyces, as shown in the chart above.

Ultrasonic Guidance
Real-time diagnostic ultrasonography (US) has been widely accepted as the imaging guidance for a dilated kidney. Overall success rates are between 88-99%, and the complication rate is low at 4-8%. The primary advantages of ultrasonographic guidance are as follows:
- Minimizes radiation exposure for patients and operating personnel
- Imaging of structures between the skin and kidney can be evaluated to determine access needle puncture depth
- No need for contrast media
- Avoids intrarenal vascular injury (color Doppler ultrasound)
- Safe for pregnant and pediatric patients
- Procedure can be performed face up (supine)
The disadvantages of ultrasonic guidance are:
- Identification of the needle requires a skilled operator
- Challenging to create an access tract when there is no or mild Hydronephrosis to dilate the kidney calyces
- Inability to visualize and manipulate a guidewire following access to the kidney.
Fluoroscopy
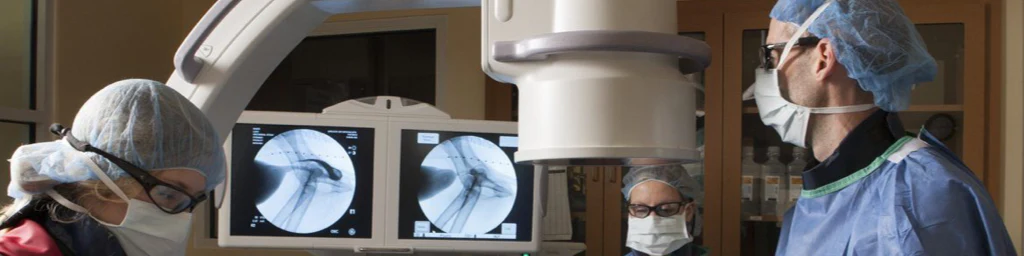
The high quality of current C-arm fluoroscopic equipment (see picture above) and the familiarity among Urologists has led to Fluoroscopy being the preferred imaging modality for puncture guidance. Surgeons prefer fluoroscopic guidance for the clear visibility of the needle and guidewire it provides. In Percutaneous Nephrolithotomy (PCNL), Fluoroscopy is very important and is used during the entire procedure. The advantages o fluoroscopic guidance are:
- Most Urologists are familiar with the equipment
- Can visualize radiopaque kidney stones
- Iodinated contrast media can be used to aid in stone localization
- Demonstrates anatomical details
While there are significant advantages to fluoroscopic guidance, radiation safety is one of the major concerns. The maximum yearly whole-body exposure to radiation recommended by the National Council on Radiation Protection is 5 rem (50 mSv). The radiation dose exposure depends on time, distance, and shielding. Ideally, the fluoroscopic time should be as minimal as possible.
Young children are more radiosensitive, and radiation exposure has been linked to malignancies, including thyroid cancer and leukemia. Therefore, radiation should be minimized in this specific group of patients.
The kidney can be opacified with contrast following placement of a catheter in the ureter or by injection of intravenous contrast material. The two methods of establishing access to the kidney are “triangulation” and the “eye of the needle or Bull’s eye” techniques. The choice of the method depends on the experience of the Surgeon. There is no difference between fluoroscopic time, operative time, hospital stay duration, complication rate, and success rates between these two approaches.

CT, MRI, & Robotic Assisted Guidance
Computed tomography (CT) guidance is another alternative that can be used for complex cases. This imaging guidance is essential in individuals with specific medical conditions such as:
- Morbid obesity (BMI> 30)
- Splenomegaly (enlarged spleen)
- Hepatomegaly (enlarged liver)
- Severe skeletal anomalies like scoliosis or kyphosis
- Patients with previous major intro-abdominal surgery
- Patients with minimal or no dilation of the renal pelvis.
Magnetic Resonance Imaging (MRI) guidance has the advantage of no radiation exposure. However, the use of MRI for kidney access is limited. The development of new MR scanner technology with faster scanning and better physical access to patients may increase its use with time.
Clinical application of robotic-assisted Percutaneous Nephrolithotomy (PCNL) is limited due to its complicated technology. The depth and angulation of the percutaneous access tract to the collecting system are controlled on fluoroscopic or CT-based data. Standard C-arm Fluoroscopy can enhance proper needle position with a visible laser guidance system.

Endoscopic Guidance
Ureteroscopic equipment, including flexible scopes, is widely available and allows for Ureteroscopy (URS) to be performed. Using the same principle, flexible ureteroscopy-assisted retrograde nephrostomy is a new option for accessing the kidney in a non-dilated collecting system. The advantages of this technique are:
- Continuous visualization for the Surgeon of all steps involved in the (PCNL) process
- Less radiation exposure
- Less bleeding
- Shorter procedure times (especially in patients with non-dilated collecting systems)
When using Ureteroscopic-assisted Percutaneous Nephrolithotomy (PCNL), access to the kidney is achieved under fluoroscopic guidance. But, the tip of the needle is visualized and monitored by Fluoroscopy and endoscopy. Then, the guidewire can be placed through and through.

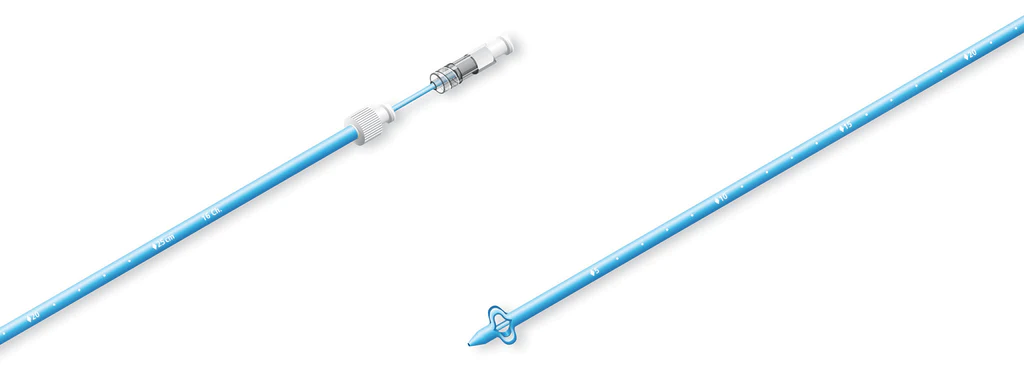
TRACT DILATION
Traditionally, tract dilation (widening of the puncture) is accomplished using successive Amplatz or Alken dilators. However, these dilators have recently been replaced by balloon dilators (shown above). Balloon dilators work by rapidly widening with a single balloon compared to the successive use of dilators to obtain the desired tract width. Some believe that balloon dilation may result in more minor trauma for the kidney.

NEPHROSCOPES
Nephroscopes are the optical instrument used by Urologists to visualize the interior of the kidney. Depending on the situation, two types could be used, rigid or flexible.
The standard rigid nephroscope (shown above) has many advantages and disadvantages, mostly around its size. Standard rigid nephroscope requires the access tract to be dilated to 30 Fr (roughly 1cm in diameter – see chart below). The large diameter of this scope provides excellent visibility and allows for proper irrigation flow around the nephroscope. The standard nephroscope also allows for Percutaneous Nephrolithotomy (PCNL) instruments such as lithotripters or graspers to be passed directly through it to allow for the removal of large stones.
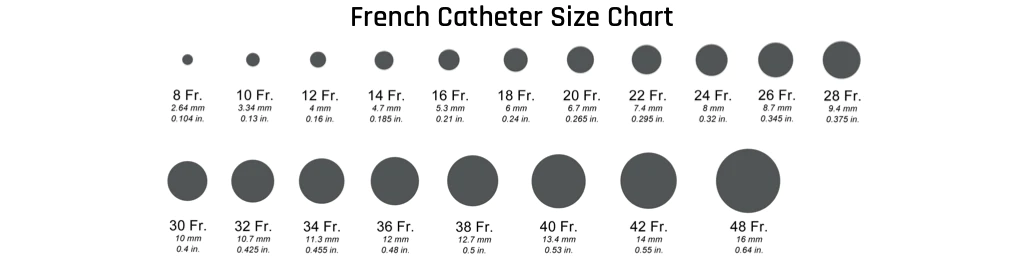
The 30 Fr access tract also allows for the removal of larger kidney stones intact, allowing for much faster stone removal when compared to removing multiple smaller fragments. However, this large access tract can result in more trauma for the kidney, creating a higher risk of complications during and after the procedure. Larger access tract sizes have also been associated with increased post-operative pain and the subsequent need for strong pain medications like opioids.
On the other hand, a flexible nephroscope provides a convenient way to visualize the interior of the kidney without the need for another access tract. Using a standard flexible cystoscope, Urologists can survey the renal pelvis and most of the kidney. They can even perform laser lithotripsy and use stone baskets to extract small residual stones, just like with Ureteroscopy (URS).
Endoscopic Combined Intrarenal Surgery (ECIRS)
The use of a ureteroscope during Percutaneous Nephrolithotomy (PCNL) has several benefits, especially for larger stones. Typically with larger stones, multiple access tracts or a two-step procedure are required to obtain complete stone fragmentation. Using only one percutaneous access tract in a one-step PCNL, combined with flexible Ureteroscopy (URS), it is possible to minimize complications without sacrificing the quality of stone fragmentation or clearance of complex stones.
The flexible ureteroscope contributes to the success of this procedure type in many ways. It has a preliminary diagnostic and intra-operative role in helping Surgeons make real-time procedural choices. It can reach calyces that are difficult or even impossible to reach with a rigid nephroscope. It actively contributes to achieving endoscopic vision and to stone fragmentation. It also reduces radiation exposure. At the end of the operation, evaluating the calyces system for residual fragments is also helpful. An additional benefit of Endoscopic Combined Intrarenal Surgery (ECIRS) is that a stone located in a calyx that is awkward for a ureteroscope to access may be passed to the nephroscope for stone fragmentation. This is called “passing the ball” (shown above).
Endoscopic Combined Intrarenal Surgery (ECIRS) in the Galdakao-modified supine Valdivia (GMSV) position has also been shown to offer good results in the treatment of impacted proximal (upper) ureteral stones (stones located in the ureter). The use of a combined approach creates an open, low-pressure system that reduces the absorptions of irrigation fluid into the circulation. This makes it possible to push the stone and/or stone fragments up into the renal pelvis, where they can be removed through the percutaneous access. In turn, this reduces the risk of ureteral injury associated with lithotripsy and stone basking.
TECHNIQUE VARIATIONS
Conventional Percutaneous Nephrolithotomy (PCNL) requires an access tract of 24-30Fr, and lithotripsy is traditionally performed using a rigid probe. The fragmentation device is usually ballistic, ultrasonic, combined, or laser fragmentation. Compared with the laser technique, ballistic and ultrasonic disintegration require straight access to the kidney stone.
Tract: Size of the surgical opening made to allow access to the kidney for various instruments measured using the “French” (Fr) size system, which refers to the outer circumference of the instrument in millimeters.
Miniaturized Percutaneous Nephrolithotomy (Miniperc) is usually classified as using tract sizes of 14-20Fr. A laser entry source generally performs lithotripsy. But, other methods are possible. Miniperc does not require a post-operative nephrostomy tube placement, leading to shorter hospital stays, less post-operative pain, and faster recovery.
Ultra-mini or Micro Percutaneous Nephrolithotomy uses a 4.85 Fr all-seeing needle with a 16-gauge needle sheath. Additionally, a three-way connector that allows irrigation and a flexible telescope, and laser fiber are used.
Conventional Vs. Mini Percutaneous Nephrolithotomy (Miniperc)
Lithotripsy devices for Miniaturized Percutaneous Nephrolithotomy (Miniperc) consist of lasers, ballistic, and dual-modality lithotripters. Traditionally, Holium lasers have been used, applying the so-called “Vacuum Cleaner” effect for fragment clearance. However, since the probes of the dual-modality lithotripters have to be down-sized in Miniperc, there is a risk that fragments will block the hollow probes.
When comparing clinical outcomes between mini and conventional Percutaneous Nephrolithotomy, outcomes such as stone-free rates, operative times, costs, and need for additional treatment need to be considered. Karakan et al. conducted a randomized trial comparing Ultra-Mini Percutaneous Nephrolithotomy and found comparable stone-free rates for kidney stones less than 2.5cm. In this study, lithotripsy was performed by Holium laser in the Ultra-Mini Percutaneous Nephrolithotomy group, and ballistic lithotripsy was used for the conventional Percutaneous Nephrolithotomy (PCNL) group. The stone-free rates were 88% for Conventional Percutaneous Nephrolithotomy (PCNL) and 89.3% for the Ultra-Mini Percutaneous Nephrolithotomy, indicating similar efficiency for the two methods.
In a randomized study performed by Song et al., Miniperc (16 Fr tract) using laser and suction was assessed compared to combined ballistic and ultrasonic lithotripsy applied in conventional Percutaneous Nephrolithotomy (PCNL). The results showed that after one procedure, the Miniperc technique was more efficient than conventional Percutaneous Nephrolithotomy (PCNL). Stone-free rates after the single procedure were 89% for the Miniperc technique and 58% for the conventional PCNL. Stone-free rates were evaluated by plain abdominal radiography (x-ray) 3-5 days after surgery. The Miniperc procedures with suction were also faster than the conventional PCNL.
In another investigation, Mini Percutaneous Nephrolithotomy using laser lithotripsy was compared with conventional Percutaneous Nephrolithotomy (PCNL) using combined ballistic and ultrasonic lithotripsy for stones larger than 2cm. Both techniques were found to be equally effective, regardless of single or multiple calyces stones.
Focusing on staghorn kidney stones, a study conducted by Zhong et al. studied individuals that were randomized to either Mini Percutaneous Nephrolithotomy or conventional Percutaneous Nephrolithotomy (PCNL). The data obtained showed that Miniperc with multiple tracts was more effective than a standard PCNL with a single tract. In short, Miniperc has a higher stone-free rate of 89.7% compared to the 68% for conventional PCNL and was associated with fewer additional treatments.
In a meta-analysis including eight trials with a total of 749 individuals, Mini Percutaneous Nephrolithotomy was compared to conventional Percutaneous Nephrolithotomy (PCNL). The authors found no difference in stone-free rates. However, the Miniperc individuals have shorter hospital stays and fewer blood transfusions than the patients in the conventional PCNL group. On the other hand, operative time was longer for the Miniperc group.
Miniaturized (Miniperc) Vs. Micro (Microperc) Percutaneous Nephrolithotomy
Percutaneous Nephrolithotomy (PCNL) has been widely used to treat kidney stones since 1970. Unfortunately, its high stone-free rate is accompanied by a more significant number of complications such as blood loss and pain, which can be reduced by decreasing the diameter of the percutaneous tract. To minimize the complications resulting from conventional Percutaneous Nephrolithotomy (PCNL), Miniperc (10-20Fr) and Microperc (4.85Fr) are now being implemented.
Both Miniperc and Microperc have been used equally effectively to treat kidney stones. To dig into this comparison deeper, we will look to a 2021 study conducted by Gao et al. in China. Data from this study shows that Microperc could produce stone-free rates comparable with that of Miniperc. But, the complications such as hemoglobin drop and urinary infections associated with Microperc were lower. It was also found that Microperc required a shorter hospital stay and operative time than Miniperc. The advantage of Miniperc over Microperc is that a flexible or rigid nephroscope can be moved through the sheath, and the lithotripsy can be continued when fragments move into other calyces.
Miniaturized Percutaneous Nephrolithotomy was initially used in 1997 to treat kidney stones in children. Jackman et al. later developed this technique for use in adults. Miniperc usually refers to a percutaneous nephroscope with a nephrostomy tract < 20Fr. Previous studies have confirmed that conventional Percutaneous Nephrolithotomy (PCNL) complications can be reduced by decreasing the diameter of the percutaneous tract. In addition, Miniperc can produce stone-free rates comparable with that of conventional Percutaneous Nephrolithotomy with lower rates of complications such as blood loss and pain. Retrograde Ureteroscopy (URS) is another procedure for treating upper urinary tract stones. Multiple studies have shown that Miniperc provides for higher stone-free rates than Retrograde Ureteroscopy. Unfortunately, Miniperc was accompanied by a higher incidence of post-operative complications.
In 2011, Desai et al. first used Micro Percutaneous Nephrolithotomy (Microperc) to fragment kidney stones. The tract of Microperc is smaller than that of Miniperc or conventional Percutaneous Nephrolithotomy (PCNL). And the puncture and lithotripsy can be completed in one step. The see-through needle helps the Surgeon puncture into the desired calyx. Microperc is widely used for medium-sized kidney stones and can produce stone-free rates of 93%. For lower pole stones, the stone-free rate of Microperc can reach 85.7%. Microperc can have a stone-free rate as high as Miniperc but lower blood loss and hospitalization time. Compared to Retrograde Ureteroscopy (URS), Microperc produced significantly higher stone-free rates. However, Microperc was accompanied by a more significant drop in hemoglobin and more extended hospital stays.
For the treatment of kidney stones in children, the stone-free rate of Microperc was 93.8%. This indicates that Microperc can be used to treat children. However, the main disadvantage of Microperc is the need to pay attention to the more considerable intrapelvic pressure. Moreover, Microprec cannot exclude fragments, so it is necessary to ensure that the stones are dusted rather than fragmented to ensure passage or residual stone.
The standard for stone-free rate was no residual or asymptomatic fragments of less than 4mm. A pooled analysis from this study showed that Microperc and Miniperc were statistically similar concerning stone-free rates. This result indicates that the stone-free rate does not decrease when the tract size is reduced. Furthermore, the stone-free rate between children and adults was analyzed in sub-group analysis, and no difference was found.
Overall, this study concluded an overall stone-free rate of 87.29% for Microperc and 86.59% for Miniperc. The stone-free rates for lower pole kidney stones were also similar. These results show that both Microperc and Miniperc are very effective in treating moderately sized kidney stones.

SAFETY
To perform Percutaneous Nephrolithotomy (PCNL) safely, it is necessary to have the appropriate endoscopic vision, cooling of the lithotripter environment to prevent overheating, and sufficient expansion of the collecting system for atraumatic movements. There is also a need to evacuate the stone fragments effectively.
Maintaining control over infrarenal pressure is essential. There is evidence that high infrarenal pressure during Percutaneous Nephrolithotomy (PCNL) increases the risk of post-operative complications. Furthermore, a rise in such pressure may cause reduced renal blood flow, pyelovenous backflow, and pyeloilymphatic backflow, which may potentially cause infectious and bleeding-related complications.
Increased infrarenal pressure leads to fluid extravasation, potentially leading to post-operative pain. Therefore, the risks and complications of intrarenal reflux, pelvic perforation, thermal injury, and serious infectious and bleeding complications need to be thoroughly evaluated and compared to conventional Percutaneous Nephrolithotomy (PCNL).
Fluid Extravasation: The leakage of blood, lymph, or other fluid from a blood vessel or tube into the tissue around it.
There are concerns that Mini Percutaneous Nephrolithotomy may cause higher intrarenal pressures due to less efficient drainage of irrigation fluid. A study by Tepler et al. found significantly higher infrarenal pressure in Miniperc procedures than in conventional PCNL. However, outcomes in both were similar in terms of complications and stone clearance.
Chu et al. explicitly focused on the differences between conventional and Mini Percutaneous Nephrolithotomy. They found comparatively higher infrarenal pressures for the Miniperc. It was also noted that the Miniperc was also more likely to be associated with post-operative sepsis. Suction through the sheath of other infrarenal pressure relating systems may overcome the concerns regarding infrarenal pressure in Miniperc.

LITHOTRIPSY
Lithotripsy is the physical destruction of hardened masses like kidney stones. In Percutaneous Nephrolithotomy (PCNL), the fragmentation device is usually ballistic, ultrasonic, or combined. Although, laser fragmentation has recently gained in popularity. Compared with the laser technique, ballistic and ultrasonic disintegration have the disadvantage of requiring straight-line access to the stone.
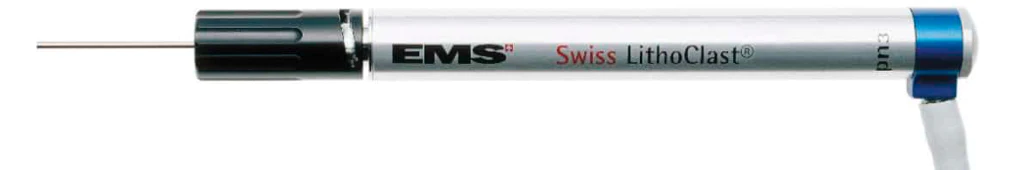
Ballistic Lithotripsy
Ballistic lithotripters use compressed air to accelerate a projectile inside the handpiece. The projectile hits the probe to elicit a shockwave that moves through the probe to the stone to cause mechanical fragmentation. Unfortunately, this leads to significant retropulsion of the stone. As such, the stone must be pushed up against the wall of the kidney’s collecting system to optimize fragmentation and avoid the loss of fragments.
Retropulsion: backward movement of kidney stones into the kidney caused by forces applied by lithotripter.

Ultrasonic Lithotripsy
Ultrasonic lithotripters use piezoceramic crystals that convert electrical energy into mechanical energy, creating ultrasonic waves at 23-25 kHz. Acoustic waves from the handpiece cause the tip to vibrate, and fragmentation is achieved when the probe tip comes into contact with the kidney stone.
Ultrasonic probes are hollow and require continuous irrigation. The irrigation fluid and tone fragments are suctioned out through the probe, which has a cooling effect on the probe and handpiece to prevent overheating.
A randomized controlled trial performed by Radar et al. in 2017 compared the safety and efficacy of ultrasonic and ballistic lithotripsy in Percutaneous Nephrolithotomy (PCNL). No significant difference was found regarding stone-free rates or complications. However, a significantly shorter stone clearance time was observed when using ballistic lithotripsy for dense stones and ultrasonic lithotripsy for weaker density stones. Thus, it seems that these two probes have advantages for different types of stones, leading to the development of combination probes, as we will discuss below.
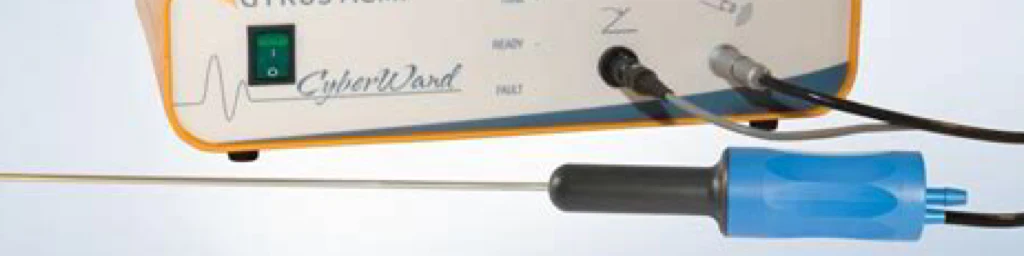
Two-Probe Dual-Modality (Ballistic & Ultrasonic) Lithotripsy
Dual-modality lithotripsy combines an ultrasonic device with a ballistic component to exploit the benefits of both devices. This allows for improved efficiency and versatility. In combined devices, the two probes are connected to a single handpiece. The inner probe can be activated alone or in conjunction with the outer probe. Direct contact with the stone is required for fragmentation with this device.

Single-Probe Dual-Modality (Ballistic & Ultrasonic) Lithotripsy
Single-probe devices have only been around since 2014. They are a dual-action lithotripsy system that uses constant ultrasonic wave energy with intermittent ballistic shockwave energy. Buttons control the device on the handpiece or by foot pedals. The probes are generally larger in single-probe devices and are hollow. The hollow aspect makes equipping these systems with suction systems a no-brainer.
Laser Lithotripsy
Lasers have become a fundamental aspect of the surgical management of kidney stones. However, their application in Percutaneous Nephrolithotomy (PCNL) is only just starting to develop. The current gold standard is the Holmium: Yttrium-Aluminum-Garnet (Ho: YAG) laser. However, there is much buzz around the new Thulium fiber laser (TFL).
COMPLICATIONS

Bleeding
The incidence of complications associated with Percutaneous Nephrolithotomy (PCNL) is 15%. Bleeding is one of the most serious complications. In a global study analysis, the incidence of bleeding was 9.4%. And while most bleeding can be treated conservatively, there is still severe bleeding in around 1% of individuals who undergo PCNL. Therefore it is crucial to identify the risk factors that may affect the incidence of bleeding and take steps to prevent bleeding.
In the scientific literature, stone size has been identified as a risk factor for bleeding during Percutaneous Nephrolithotomy (PCNL). Since the goal of PCNL is to remove stones, Surgeons must reach into all corners of the kidney, which may tear the neck of the kidney calyx and result in bleeding. Large kidney stones also add to the operative time, leading to increased complications.
The type of stone is also a risk factor for bleeding during Percutaneous Nephrolithotomy (PCNL). Stones that are present across two or more calyces are defined as Staghorn stones. Because the outer layer (cortex) in Staghorn stones is denser, the access channel is longer. Thus individuals with Staghorn stones are more prone to bleeding.
The degree of Hydronephrosis is another factor that can impact bleeding. In patients with no or mild Hydronephrosis, the outer layer of the kidney (cortex) is relatively thick. This is because as the degree of Hydronephrosis increases, the distribution of renal vessels gets spread out as the kidney stretches to accommodate the back-up of urine. Otherwise, in normal circumstances, the kidney cortex is condensed and thicker than it would be if it were stretched out due to urine back-up. When not stretched out due to Hydronephrosis, the risk of bleeding is higher due to the greater concentration of renal vessels.
Infections
It has been reported that up to one-third of patients might experience some pre-operative complications after Percutaneous Nephrolithotomy (PCNL). Especially fever and urinary tract infections, constituting about 21-39.8% of all complications. Infection is potentially devastating and the leading pre-operative cause of death among them.
Since its introduction, Percutaneous Nephrolithotomy (PCNL) is still the most commonly performed surgery for age and complex kidney stones. Though the safety and efficacy of the procedure have been well-defined, infectious complications are still dangerous. In addition, post-operative infectious complications were associated with prolonged hospitalization and additional antibiotic treatments.
Post-Percutaneous Nephrolithotomy (PCNL) complications are more commonly found in patients with a history of pre-operative Urinary Tract infections (UTI), previous history of renal surgeries, large stone burden, operative times greater than 90 minutes, and the presence of residual stones. The number or size of the percutaneous tracts was not associated with significant risk.
Urosepsis is a rare but life-threatening complication that can occur after Percutaneous Nephrolithotomy (PCNL). Urosepsis is a dysregulated systemic inflammatory response to urogenital infection. Generally, it occurs secondary to the distribution of previously localized uropathogenic bacterial infection into the bloodstream. Patients who experience urosepsis have mortality rates of 20-40%, which increases to 50% in patients who experience refractory septic shock. Given the high mortality rates, investigation into predictive factors for urosepsis in struvite stone patients receiving treatment is needed.
As such, several different criteria have been developed to identify patients at high risk for developing sepsis, including the Inflammatory Response Syndrome (SIRS) criteria. SIRS is a composed constellation of symptoms which include:
- Fever ≥ 100.4℉ (38℃)
- Tachycardia >90 beats per minute
- Tachypnea > 20 breaths per minute
- Elevated white blood cell count > 12,000/dL
The most recent classification system, known as the Sequential (sepsis-related) Organ Failure Assessment (SOFA), was introduced by the Third international Sepsis Consensus Definition Task Force. With this new classification, a bedside quick-SOFA (q-SOFA) scoring system was also adapted to facilitate the diagnosis of sepsis. This q-SOFA scoring system classified patients at high risk of progressing to sepsis if at least two of the following criteria are met:
- Glasgow Coma Scale (GSC) < 15
- Systolic blood pressure of ≤ 100mmHg
- Tachypnea of ≥ 22 breaths per minute
The q-SOFA scoring system was shown to have higher specificity and positive predictive value than the SIRS criteria in identifying sepsis cases in a multi-institutional Endourologic Disease Group for Excellence (EDGE) Research consortium study.
Currently, the available literature has documented risk factors for sepsis in patients with urinary stones following Percutaneous Nephrolithotomy (PCNL). These risk factors include pre-operative bacteriuria, stone size, and operative time. In particular, to struvite stones treated with Percutaneous Nephrolithotomy (PCNL), their inherent infectious nature and the presence of pre-operative multi-drug resistant (MDR) bacteriuria have been identified as variables that may predict sepsis post-operatively.
Stone Migration
Antegrade migration (with the flow of your urine) of residual stone fragments into the ureter after Percutaneous Nephrolithotomy (PCNL) is rare. However, stone-related events resulting from obstructions caused by residual fragments may require additional procedures to remedy, such as stunting or Ureteroscopy (URS). These events prolong hospital stays, delay nephrostomy tube removal, and increase costs.
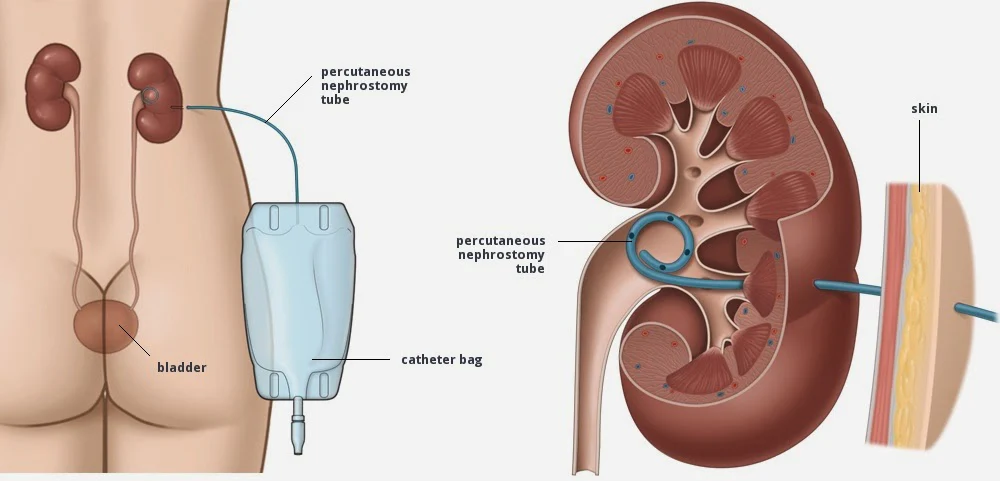
Urinary Leakage
Despite high success rates, Percutaneous Nephrolithotomy (PCNL) involves many complications such as urinary leakage. Urinary leakage from the nephrostomy tube site in conventional PCNL procedures was present in roughly 50% of patients based on a pooled analysis of studies. Nephrostomy tubes (discussed in more detail in the next section) help maintain homeostasis and prevent urine leakage, thus, preventing the development of urinomas (a mass formed by encapsulated urine). However, urine leakage from the drain site after removing the post-operative nephrostomy tube is a common problem.
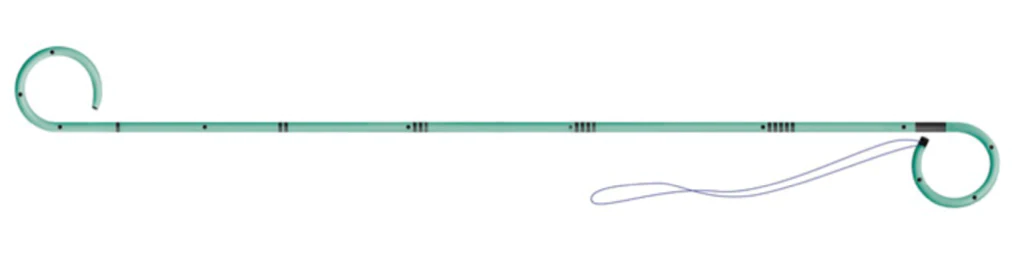
Post-operative Double J (JJ) stents are recommended for patients who are at an increased risk for prolonged urinary leakage.
EXIT STRATEGIES
Post-operative renal drainage has evolved over time with a trend towards leaving smaller nephrostomy tubes and even some Urologists leaving individuals completely tubeless. In general, there are three main categories:
- Large nephrostomy tube drainage
- Small nephrostomy tube drainage
- Tubeless drainage (ureteral stent or catheter instead of nephrostomy tube)
The large nephrostomy tube of choice is the 24 Fr (8mm diameter) malecot re-entry nephrostomy tube. This size is appropriate for the access tract during traditional Percutaneous Nephrolithotomy (PCNL). The larger diameter also provides low-pressure direct drainage of the kidney. The malecot (see photo below) sits comfortably in the renal pelvis, helping to keep the tube in place. The ureteral portion of this tube allows for quick access in cases where multiple staged procedures are necessary. Thus, this tube size is preferred for large stone sizes.
Recently, an effort has been made to use smaller diameter nephrostomy tubes when possible. Small nephrostomy tubes have been associated with decreased post-operative pain and prescription pain medication use. Different tube sizes can be used, ranging from 8.5 Fr (~2.75mm diameter) to 14 Fr (4.67mm diameter). In addition, small nephrostomy tubes are a safe alternative for drainage in uncomplicated cases.
Tubeless Percutaneous Nephrolithotomy (PCNL) has recently become more popular and has been proven to be safe. There are two ways to achieve drainage when considering tubeless drainage: Double J (JJ) Stent or a Foley catheter. When using a Double J (JJ) stent, the Foley catheter is removed 24 hours after surgery. The Double J (JJ) stent is removed 5-10 days later. When using a ureteral catheter, both the Foley catheter and ureteral catheter are removed 24-48 hours after surgery. The tubeless approach to drainage has also been shown to decrease post-operative pain, shorten hospital stay time, and reduce recovery time. Therefore, it is recommended that tubeless PCNL be reserved for straightforward, uncomplicated cases.

POST-OPERATIVE CONSIDERATIONS
Antibiotics
There are no clear guidelines for post-operative antibiotic use. However, these cultures should guide antibiotic choice in individuals with positive urine or stone cultures. Individuals with post-operative fevers and sepsis should be treated according to their clinical condition.
Stents
Post-operative Double J (JJ) stents are recommended for patients who are at an increased risk for prolonged urinary leakage.
Imaging
Any surgical treatment for kidney stones aims to obtain stone-free status. However, the cut-off level for what represents “stone-free” and the imaging technique used varies depending on the urological center. In addition, complete removal of all stone fragments is critical to preventing the recurrence and regrowth of stones. This makes post-operative imaging for residual fragments necessary.
X-Rays are one of the most commonly used imaging modalities to detect residual fragments following Percutaneous Nephrolithotomy (PCNL). The main advantages of the X-ray modality are its low cost and lower radiation exposure (~0.15 mSv). Additionally, most kidney stone types are visible on X-ray (except uric acid).
Ultrasound (US) is non-invasive and does not utilize radiation. It can be used to directly visualize residual fragments in the upper collecting system of the kidney as small as 2mm. Ultrasound can also provide information on the dilation of the kidney’s collecting system. However, routine follow-up with only Ultrasound to identify residual fragments after PCNL is not advised. The imaging sensitivity is directly affected by the presence of a nephrostomy tube and other post-operative debris.
Computerized Tomography (CT) is currently the imaging modality of choice for evaluating the stone-free status and identifying residual fragments after Percutaneous Nephrolithotomy (PCNL). Sensitivity and specificity are generally above 90% for all stone types.
Optimal timing for post-operative imaging is also debated between urological centers. In many centers, imaging is performed routinely at post-operative day 1. However, this can potentially be associated with false-positive results due to post-operative stone dust. Additionally, false positives will be identified for any residual fragments that remain that may have passed spontaneously without incident.
As a result, it is recommended that imaging be completed at the end of the first month after surgery.

CONCLUSIONS
In current times, Percutaneous Nephrolithotomy (PCNL) is still not standardized in terms of technical considerations such as access tract size and devices used in stone destruction. Conventional Percutaneous Nephrolithotomy (24-30Fr) enables the use of probes that make it possible for fragments to be both disintegrated and removed by suction through the same probe. Older devices that rely purely on ballistic or ultrasonic techniques are still viable and have proven their efficacy and safety over many years. New technological advances inclusion single-probe dual-modality lithotripters are promising. They seem to be more effective than single energy probes.
Mini Percutaneous Nephrolithotomy (PCNL) requires smaller probes for lithotripsy, and larger fragments cannot be extracted through the probe. However, the vacuum cleaner effect can be effectively evacuated small fragments resulting from laser lithotripsy. New developments such as the use of laser lithotripsy in combination with suction devices in Mini Percutaneous Nephrolithotomy (PCNL) seem to be safe and effective. They may even further increase the efficacy and safety of Mini Percutaneous Nephrolithotomy (PCNL). Moreover, laser probes are flexible and can be used in flexible endoscopic devices.
Unfortunately, there is limited quality evidence comparing convention Percutaneous Nephrolithotomy (PCNL) to Mini Percutaneous Nephrolithotomy. However, research has indicated that Mini Percutaneous Nephrolithotomy (PCNL) is associated with fewer bleeding complications and shorter hospital stays. However, a drawback of Mini Percutaneous Nephrolithotomy is the longer operative times. On the other hand, the use of laser lithotripsy combined with function may be a promising alternative that can potentially improve Mini Percutaneous Nephrolithotomy performance by shortening operative times.
In that context, using supine positioning of patients during Percutaneous Nephrolithotomy (PCNL) is a good alternative, especially in complex renal stone situations that require a combined approach (Endoscopic Combined Intrarenal Surgery- ECIRS). However, there is no evidence that one method is better than the other, such as conventional Percutaneous Nephrolithotomy (PCNL) with ballistic and/or ultrasonic disintegration or Mini Percutaneous Nephrolithotomy with laser disintegration. However, the evolution of different techniques has increased the possibilities of a personalized approach. In other words. The suitable method for the right patient.

Comments or questions?
Responses