Published: April 14, 2024 | 1 min read
Can Diabetes Cause Kidney Stones?
ARTICLE SHORTCUTS
- WHAT IS DIABETES?
- HOW IS DIABETES LINKED TO KIDNEY STONES?
- WHY DOES DIABETES LEAD TO ACIDIC URINE?
- IS DIABETES LINKED TO CALCIUM STONES?
- CAUSES OF DIABETES
- HOW TO MANAGE URIC ACID STONES AMONG DIABETICS?
- REFERENCES
Did you know that 1/3 of US adults have pre-diabetes?
Recent data from the Centers for Disease Control and Prevention (CDC) shows that around 96 million US adults have pre-diabetes, while 37.7 million have diabetes.
These are alarming numbers because this diabetes is directly linked to your risk of forming uric acid (UA) kidney stones.
Before we get deeper into its connection to kidney stones, first, let’s have a background of what diabetes is all about.
WHAT IS DIABETES?
Diabetes Mellitus, or diabetes for short, is a chronic condition that affects how the body regulates blood sugar (glucose). There are two types of diabetes.
The first type, which accounts for about 5% of all cases, is a condition in which the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. The pancreas can’t produce enough insulin, a hormone that helps glucose enter cells for energy. As a result, people with Type 1 diabetes need insulin therapy everyday.
Meanwhile, the second type is characterized by insulin resistance. The primary role of insulin is to signal the cells to accept glucose. When the cells become resistant to these signals, more sugar will end up in the blood, leading to Type 2 diabetes. Around 95% of diabetic patients have this type.
People with diabetes commonly experience these symptoms:
- Increased thirst
- Increased hunger
- Frequent urination
- Frequent infections
- Unexplained weight loss
- Fatigue
- Blurred vision
- Wounds that do not heal
- Numbness or tingling in the hands or feet
- Darkened areas in the skin (e.g., armpits and neck)
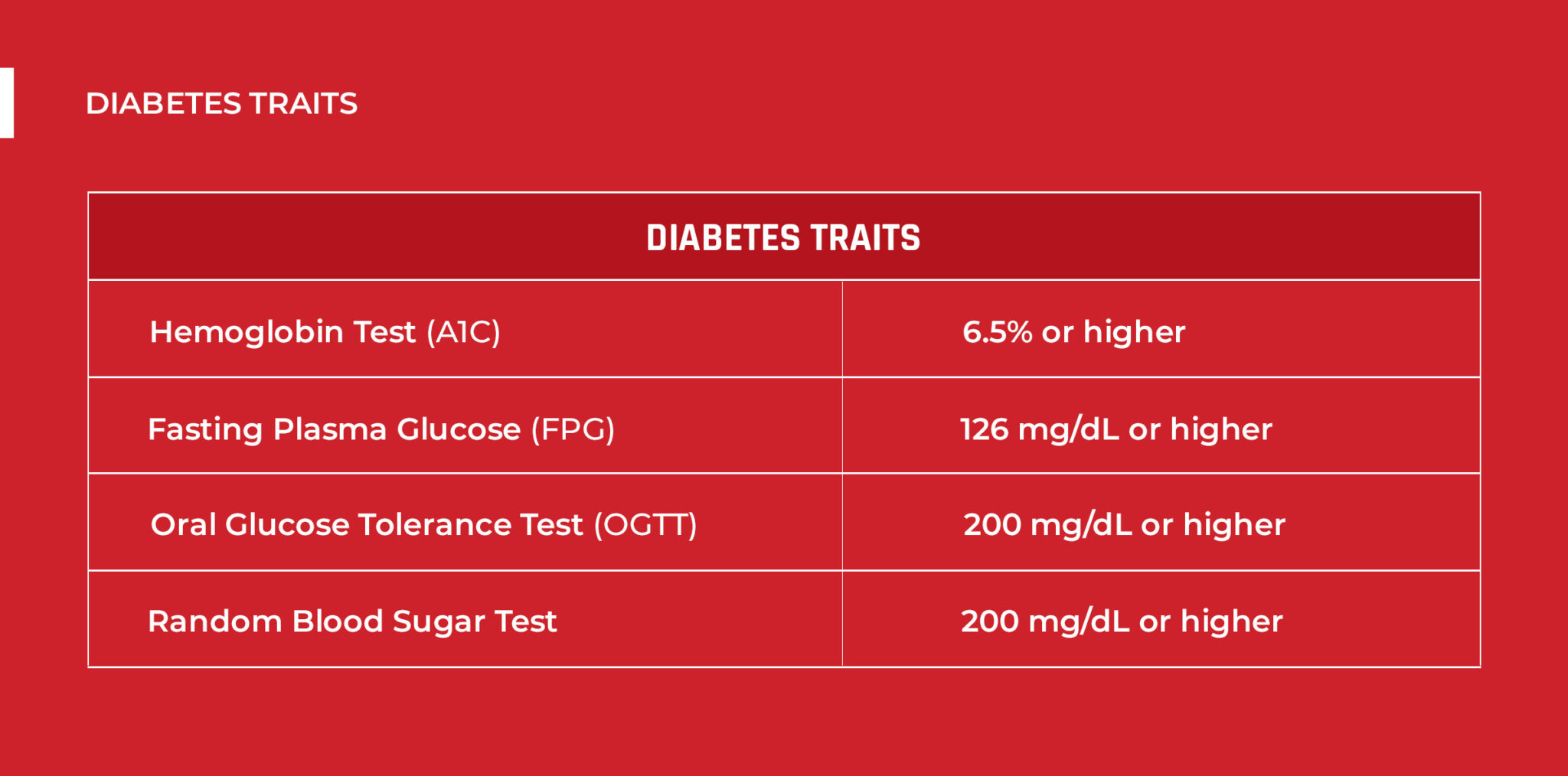
If you have one or more of these symptoms, better have a diagnosis. It is usually done through a blood test. Here are the traits you should watch out for:
Now that we have an idea of both Type 1 and 2 diabetes, let’s dig into their link to kidney stones.
HOW IS DIABETES LINKED TO KIDNEY STONES?
The risk of forming UA stones is twice as high among people with diabetes. This is true for both Type 1 and 2 patients.
Researchers examined urinary crystals in 116 patients with Type 1 diabetes. They found that uric acid crystals are 22% higher in Type 1 diabetic patients compared to 5.2% in non-diabetic subjects.
The same result was noted in a study involving 2,464 stones from 272 Type 2 diabetic patients. Compared to calcium stone-formers, more uric acid stone-formers are diabetic.
Furthermore, in a study conducted among 5,000 stone-formers, researchers found that 1/3 of pure UA stone-formers have diabetes. Interestingly, none of the calcium stone-formers and healthy controls were diabetic.
You might wonder – why does diabetes results in higher UA stone risk?
Type 1 and 2 diabetes cause an acidic urine environment (pH <5.5). Uric acid is a weak acid that is usually soluble in the urine. However, when your urine gets too acidic, uric acid crystallizes.
Western medicine blames protein-rich foods for uric acid stones due to purine content (precursor to uric acid). However, this advice is a total misinformation because uric acid isn’t to blame for this stone type. The real culprit you have to troubleshoot is acidic urine. Many studies have found that patients with uric acid stones don’t necessarily have excess uric acid. Instead, the common denominator is a urine pH of less than 6.
WHY DOES DIABETES LEAD TO ACIDIC URINE?
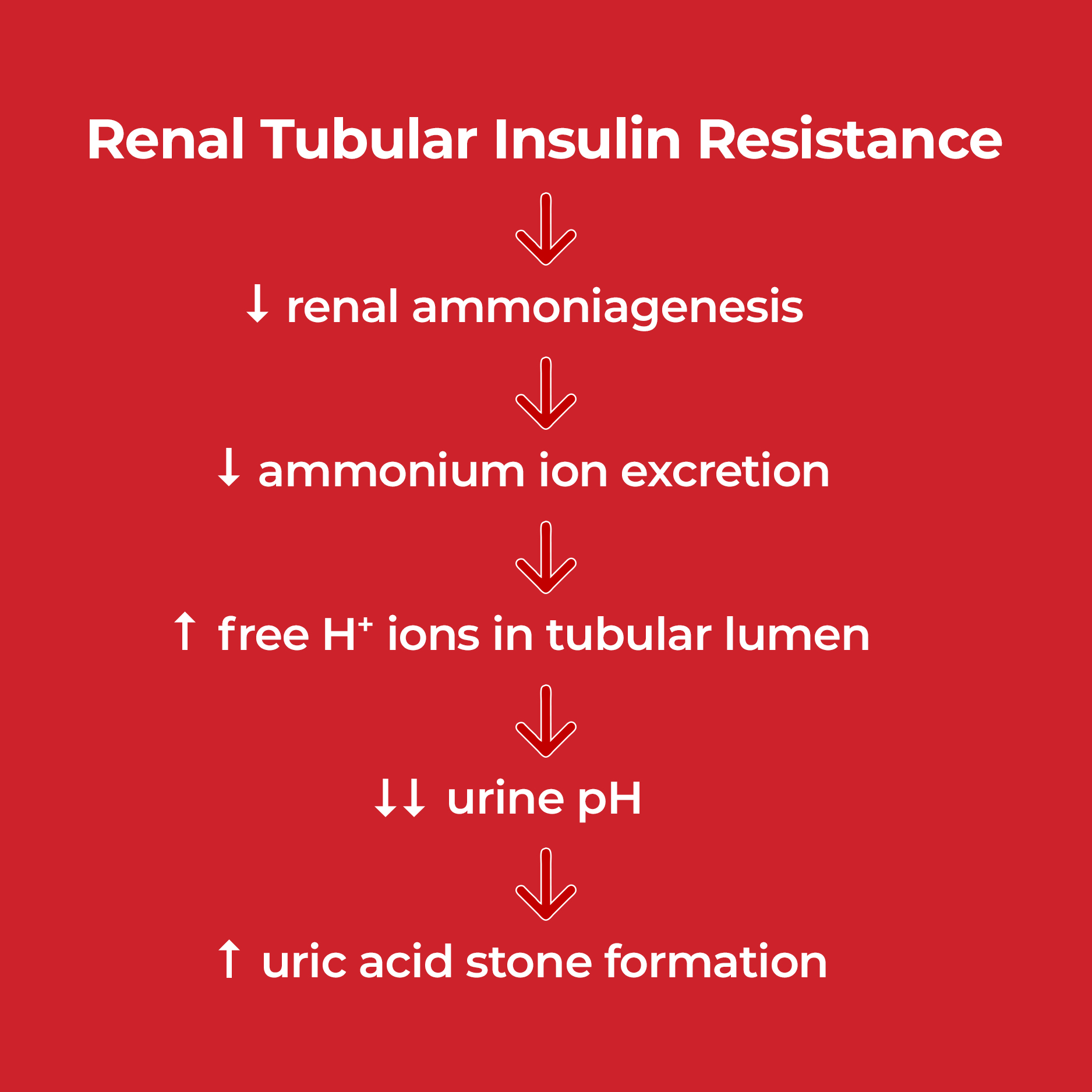
Diabetic patients have more acidic urine due to decreased ammonium in the urine. Ammonium is an alkaline ion. The kidney uses the amino acid glutamine to produce it. When a person has insulin resistance, higher levels of free fatty acids end up in the blood. These fatty acids can enter the proximal tubules (initial filtration unit) of the kidney and interfere with ammonium production. Lower amounts of ammonium can lead to lower urine pH.
IS DIABETES LINKED TO CALCIUM STONES?
Some doctors link diabetes to an increased risk of forming calcium stones. That’s because high blood sugar levels can lead to metabolic acidosis (excess acid in the blood). When there’s excess acid in the blood, the kidney will reabsorb citrate back into the bloodstream to balance the acidity. In return, less citrate will be excreted in the urine. Citrate is protective against kidney stones because it binds with calcium to prevent oxalates and phosphate from binding to it.
But honestly, for most calcium stone-formers, avoiding oxalates would solve the issue. That’s because around 90% of calcium stones (80% of all kidney stone cases) are due to oxalates. Oxalates are naturally-occurring chemicals in plants. Most plants humans eat, such as leafy greens, grains, nuts, and seeds, are rich in oxalates. So, if you avoid munching on plants, you’ll keep calcium-oxalate stones away.
CAUSES OF DIABETES
The exact origin of Type 1 diabetes is not yet fully understood. Fortunately, this type only accounts for around 5% of total cases. For the 95% who suffer from Type 2 diabetes, dietary and lifestyle factors are the primary causes.
To give you an idea of what factors contribute to your condition, take note of the following:
Poor diet
We will never get tired of telling you that diet plays the biggest role in your overall health. When you eat the wrong diet, you will cause havoc in your gut, which will lead to many diseases. That includes diabetes. The worst foods that ruin your metabolism are plant foods. There are a couple of reasons for this.
First, plant foods are rich in linoleic acid (an omega-6 fatty acid). An imbalance between omega-6 and omega-3 fatty acids is the primary cause of impaired metabolism.
But you might ask – Don’t plants contain omega-3?
It’s true that some seeds (e.g., flax seeds) are also rich in omega-3. However, the harms outdo the benefits because they are commonly high in oxalates. The best sources of both omega-6 and omega-3 are animal products because they don’t contain oxalates. You can get omega-3 from seafood, like salmon, mackerel, and sardines. Since animal products have lesser omega-6 than plants, going animal-based is also the smartest choice to avoid excesses. The best sources of this fatty acid are egg yolks, dairy and grass-fed poultry.
Also, if you keep eating plant-based diets, you’ll have the tendency to eat excess sugar and carbohydrates. If your sugar intake exceeds 36g (for men) and 25g (for women), that’s already excessive and is putting you at higher health risks. It can lead to insulin resistance and eventually to Type 2 diabetes.
Obesity
The rise of the processed food industry dramatically increased obesity worldwide. And the explanation is quite simple. Most manufacturers and restaurants shifted from using animal fats to using vegetable oils and seed oils. This resulted in high linoleic acid content in foods. Again, linoleic acid sabotages your metabolism.
Also, processed foods are commonly high in sugar. Some can be natural, like honey, molasses, maple syrup, and nectar. Others can be synthetics like anhydrous dextrose, corn syrup solids, dextrose, sucrose, and high-fructose corn syrup (HFCS). If you find these names on food labels, you know they are all sugar masqueraded to fool you. And if you are not mindful as to how much sugar you are eating, you’ll surely be in trouble.
Physical Inactivity
If you live a sedentary lifestyle, your body doesn’t burn calories. On the contrary, if you are active, you have more outlets to burn calories, which will help you maintain your weight. Also, exercising can improve the body’s sensitivity to insulin, which is crucial in preventing and treating diabetes.
Damaged Pancreas
The hormone insulin is produced in the pancreas. So, issues surrounding your pancreas, such as pancreatitis (inflammation), pancreatic cancer, and trauma, can all harm the cells that produce insulin. This can increase your risk of diabetes. One of the primary reasons our pancreas gets damaged is excessive alcohol intake. When we say excessive, it means drinking more than 2 drinks for men and more than one for women.
Medicines
Sometimes, taking certain medications can harm the cells or disrupt the way insulin works in the pancreas. These include:
- Niacin – a type of vitamin B3
- Diuretics (e.g., Thiazide diuretics)
- Anti-seizure drugs (e.g., Valproate)
- Psychiatric medications (e.g., Atypical Antipsychotics)
- Drugs to treat human immunodeficiency virus or HIV (e.g., Protease Inhibitors)
- Pneumonia medication (e.g., Pentamidine)
- Anti-inflammatory (e.g., Glucocorticoids)
- Anti-rejection medicines (e.g., Corticosteroids)
- Drugs to reduce “bad” cholesterol levels (e.g., Statins)
If you are suffering from insulin resistance and are taking any of these medications, better have a conversation with your doctor to make the necessary adjustments.
In general, if you have diabetes, consider the causes mentioned in this article. Check which of these (maybe all) are causing you diabetes. For most people, this disease is reversible, especially in the early stages. You can do that by fixing your diet and lifestyle.
HOW TO MANAGE URIC ACID STONES AMONG DIABETICS?
Uric acid kidney stones are typically a result of metabolic disorders that lead to acidic urine. Diabetes is among the most common metabolic diseases out there. So, if you want to fix this stone type for good, you must reshape your diet and lifestyle.
But if you currently have UA stones, try to pass them using CLEANSE. UA stones are less dense, meaning they easily break apart while passing. Use CLEANSE, coupled with proper hydration (around 96 oz. of water) for easier passage.
Are you opting for prevention?
There’s a way out of that sinkhole. All you need to do is focus on reshaping your diet and lifestyle. We are here to help you do that. If you want to get all the resources you need to overcome your kidney stones, check out our Coaching Program.
REFERENCES
- Diabetes
- Diabetes mellitus and the risk of nephrolithiasis
- Metabolic syndrome, obesity and kidney stones
- Study of Urinary Crystals for Type 1 Diabetics
- Symptoms & Causes of DiabetesType 2 diabetes mellitus and renal stones
- The metabolic syndrome and uric acid nephrolithiasis: Novel features of renal manifestation of insulin resistance

Comments or questions?
Responses