Published: May 5, 2024 | 9 mins read
Sjögren’s Syndrome and Calcium Phosphate Stone Link
Have you heard about Sjögren’s syndrome? It is an autoimmune disease that commonly affects the body’s moisture-producing glands and the joints.
What does it have to do with kidney stones?
You don’t want to miss this blog if you are a calcium phosphate stone-former. Sjögren’s syndrome causes a lot of trouble in your kidney, increasing your risk for this stone type.
But before we spill the beans, let’s briefly describe this not-so-famous syndrome.
What is Sjögren’s Syndrome?
Have you experienced dry, itchy, gritty eyes and a dry mouth that feels like it’s full of cotton? These are two common symptoms of Sjögren’s syndrome. You may also feel fatigue and muscle and joint pains.
This syndrome is the second most common autoimmune condition that affects the body’s joints, muscles, bones, and connective tissues. It also affects the glands that produce fluids such as saliva, sweat, and tears.
Sjögren’s syndrome has two types – primary and secondary.
Primary Sjögren’s syndrome occurs without any rheumatic diseases. Rheumatic diseases are conditions that cause the immune system to attack joints, muscles, bones, and other organs.
Meanwhile, secondary Sjögren’s syndrome forms when you have another rheumatic disease, such as:
- Rheumatoid Arthritis (RA) – Primarily affects the joints, causing inflammation, pain, stiffness, and swelling. It can lead to joint damage and deformities over time.
- Systemic Lupus Erythematosus (SLE) – Affects multiple organs and systems in the body, including the skin, joints, kidneys, heart, and lungs.
- Scleroderma – Also known as systemic sclerosis. This leads to abnormal growth of connective tissues, causing thickening and hardening of the skin and internal organs.
Now that we’ve understood Sjögren’s syndrome, let’s get to the most critical point—how is it linked to kidney stones?
Sjögren’s Syndrome and Calcium Phosphate Stones
As mentioned earlier, Sjögren’s syndrome and calcium phosphate stones are linked.
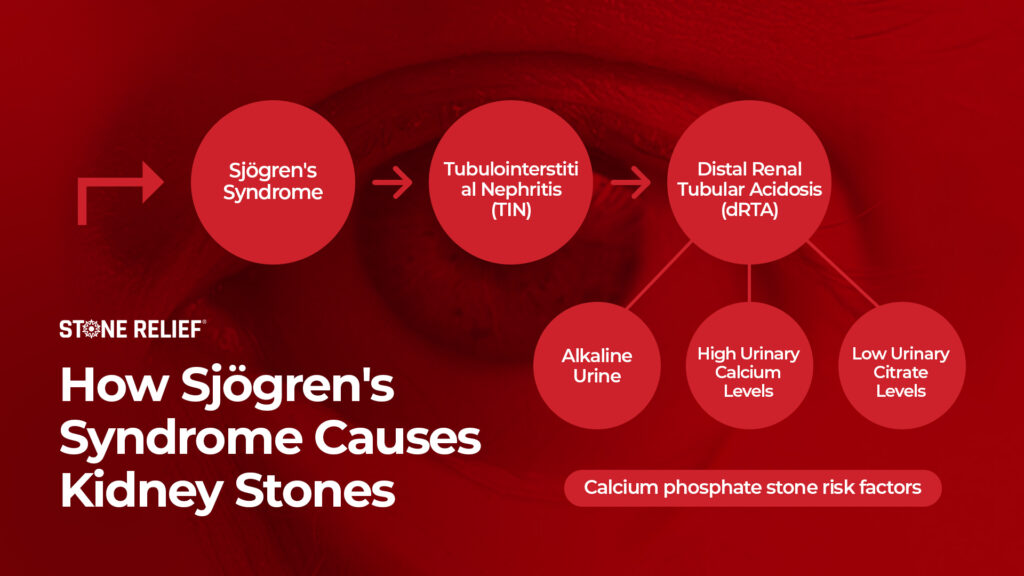
Around 14% to 25% of people with Primary Sjögren’s syndrome develop calcium phosphate stones. This stone type forms because Sjögren’s syndrome causes alkaline urine. It also promotes high calcium and low citrate levels in the urine. These three are risk factors for calcium phosphate stones.
But how does Sjögren’s syndrome cause all this trouble in the kidneys?
The following section will explain the details.
The Mechanism of How Sjögren’s Syndrome Leads to Kidney Stones
Imagine yourself making a house using domino pieces. You are carefully laying down the structure when one domino piece suddenly slips from your hand, hitting another, until the whole structure falls. That goofy domino dude best describes Sjögren’s syndrome in the kidney stone context. It can cause a series of conditions to increase your calcium phosphate stone risk.
Here are the three main reasons why it can lead to kidney stones:
1. Alkaline urine (over 7.0 pH)
Sjögren’s syndrome can cause a kidney disease called Tubulointerstitial nephritis (TIN). This is characterized by inflammation and damage to the kidney’s tubules (tiny, tube-like structures) and connective tissues.
TIN is like a trojan virus in a computer program. It can cause the kidney tubules to become dysfunctional, leading to a condition known as distal renal tubular acidosis (dRTA). dRTA happens when the kidneys fail to buffer the acidity in the blood. As a result, acid imbalance occurs. There is a decrease in the pH of the blood (acidemia) and an increase in urinary pH (alkaline urine).
Researchers don’t know the exact way Sjögren’s syndrome causes dRTA. However, studies have shown that specific pumps (H-ATPase) are missing in kidney tissues, and some patients have antibodies against carbonic anhydrase II, an essential enzyme in regulating the kidney’s acid-base balance. Both are believed to cause dRTA, which leads to alkaline urine.
Aside from alkalizing the urine, dRTA also causes another problem that directly affects stone risk: lowering citrate levels.
2. Low citrate levels in the urine
Citrate is like Ironman’s armor, shielding calcium against the bad guys. That’s because it sticks with calcium to prevent stone-forming elements from adhering to it. So, it is an important protector against calcium-based stones.
Now, here comes the conflict. dRTA can cause hypokalemia or low potassium levels. Around 30% to 47% of primary Sjögren’s syndrome patients with kidney issues develop hypokalemia.
According to researchers, low blood potassium increases the body’s acid load. This affects the NaDC protein that transports citrate. The body reabsorbs citrate to buffer the acidity in the blood. The exact mechanism of how this happens is also not fully understood.
But wait, we’re not yet done with dRTA. There’s still another reason why it’s troublesome for kidney stone-formers. It can increase your urinary calcium levels!
3. Increased calcium levels in the urine
When a person has dRTA, the kidneys cannot properly excrete hydrogen ions into the urine. Again, this leads to acid buildup in the body (acidosis). This acidosis can strip calcium off your bones, like a bully classmate pulling your pants down in elementary school. This increases calcium levels in the urine. What a jerk!
Since Sjögren’s syndrome is such a troublemaker, where the heck do you get it? In the next section, we will explore the possible causes of this syndrome.
Sjögren’s Syndrome Causes
Have you ever experienced being in trouble because a very drunk guy thought you hit him or something? In the same way, when you have Sjögren’s syndrome, your immune system acts like that drunk guy mistakenly attacking your healthy tissues instead of defending your body against infections and illnesses.
Unfortunately, doctors do not fully understand the exact reasons why the immune system starts attacking the body. However, if you pay attention to all the details we’ve shared above, we can make insightful theories.
First, Sjögren’s syndrome is an autoimmune disease not proven genetic. That means it is acquired. It surely speaks about the relationship between one’s diet and immune dysfunction.
Second, it commonly attacks the muscles, joints, ligaments, and bones. Make a guess? Mainstream media promotes going vegan, which doesn’t translate well to healthy joints!
Third, dRTA is a metabolic dysfunction related to electrolyte (calcium, potassium, sodium, etc.) imbalance. There’s a possibility that electrolyte imbalance is also playing a role in why you have dRTA since it’s not clear how Sjögren’s syndrome leads to dRTA.
If we were to describe Sjögren’s syndrome in one word, that would be “mysterious.” Imagine! It doesn’t want to conceal its actual cause! However, we firmly believe that DIET is the main culprit.
Anyway, let’s add to that confusion (What?!). Sjögren’s syndrome can manifest in different ways in the body and through various health conditions, so diagnosis is also challenging. It’s almost like playing hide-and-seek. To give you an idea of how difficult it is, hop on to the next section.
How to Diagnose Sjögren’s Syndrome?
Sjögren’s syndrome doesn’t have a single test for diagnosis. A mix of symptoms and lab findings are used to identify it.
The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) developed a classification criteria for diagnosing Sjögren’s syndrome to make things easier. These guidelines provide a standardized approach to identifying individuals who likely have Sjögren’s syndrome based on clinical features and laboratory tests.
Here are the key features of the 2016 ACR/EULAR classification criteria for Sjögren’s syndrome:
- Anti-Ro/SSA Antibody Positivity – Testing positive for autoantibodies commonly associated with Sjögren’s syndrome.
- Lymphocytic Sialadenitis – Evidence of inflammation in the salivary glands (sialadenitis) observed on a salivary gland biopsy, typically measured by a focus score of ≥1 focus per square millimeter.
- Objective Dryness: Using specific tests, such as Schirmer’s test for eye dryness and an oral test for mouth dryness.
The classification criteria assign points based on the presence of these key features. A total score of 4 or higher, with dryness in either the eyes or mouth, is considered diagnostic of Sjögren’s syndrome according to these guidelines.
Okay, let’s say you confirmed that you have Sjögren’s syndrome. How do you use that information to manage your kidney stones?
In the next chapter, we will give you tips on how to treat/prevent Sjögren’s syndrome so that it won’t cause you more calcium phosphate stones.
Strategies to Stop Sjögren’s Syndrome Causing Calcium Phosphate Stones
The best way to treat kidney issues in Sjögren’s syndrome isn’t clear yet, so treatment depends on how the disease presents.
However, if you have TIN, correcting electrolyte imbalances is important. Should you do it with synthetics? Nope. The body recognizes synthetics as garbage. They don’t help at all. The best way to correct your electrolyte imbalances is through DIET. That’s why we invite you to join our Coaching Program. Two heads are better than one; it’s easier to solve your diet issues when an expert guides you. Also, you need to strengthen your immunity because how else would you defeat an acquired autoimmune disease? Again, synthetics are not the way. They are like rusty bolts that snap easily with one kick when robbers try to break into your lovely home. They are not helpful at all. You need to strengthen your immune system through proper DIET.
If you believe we could be the right guide to help you fix your diet, secure a spot in our Coaching Program, and we will help you assemble a diet plan to manage Sjögren’s syndrome and its domino effect on kidney stones.
REFERENCES

Comments or questions?
Responses
WHAT TO READ NEXT
Publish Date: June 23, 2024
Do You Have a Phosphate Leak Leading to Kidney Stones?
Publish Date: June 9, 2024
The #1 Genetic Cause Of Kidney Stones: Cystinuria Disease
Publish Date: May 26, 2024
Distal Renal Tubular Acidosis Leads To Calcium Phosphate Stones