Published: May 12, 2024 | 7 mins read
Hyperparathyroidism Impact on Kidney Stones – Calcium Deficiency Alert!
The parathyroid glands are really small but can be troublesome!
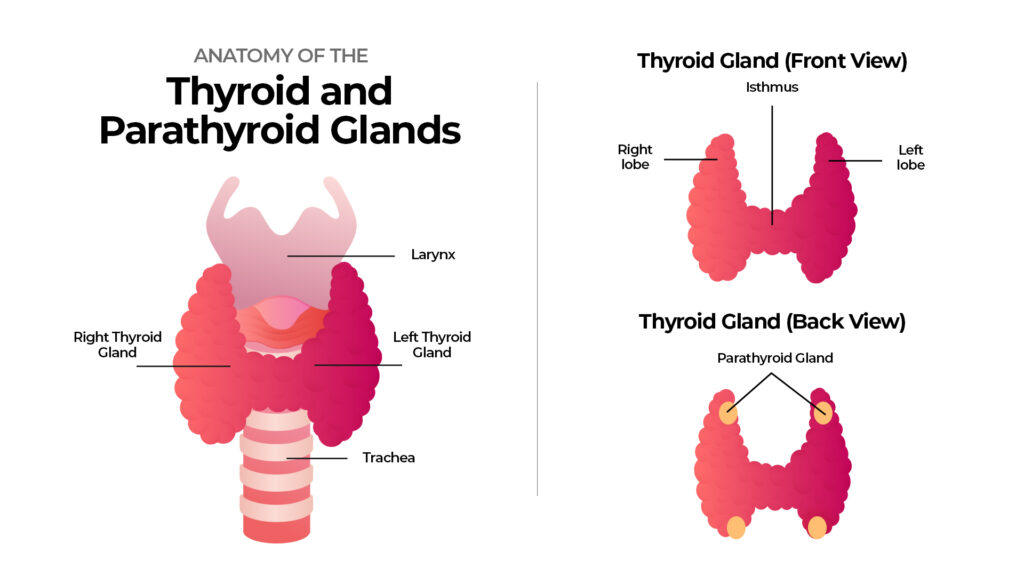
If you are unfamiliar with these glands, they are four small glands (the size of a pea) in your neck area. Their primary function is to regulate calcium levels in your body by producing parathyroid hormones (PTH).
Suppose your parathyroid glands produce abnormally high PTH (a.k.a. hyperparathyroidism). In that case, it leads high calcium levels in the urine, which can contribute to kidney stone formation if you have other factors, which we will cover in this blog. So, make sure to read on! In the meantime, let’s give a little background to what hyperparathyroidism is about.
What is Hyperparathyroidism?
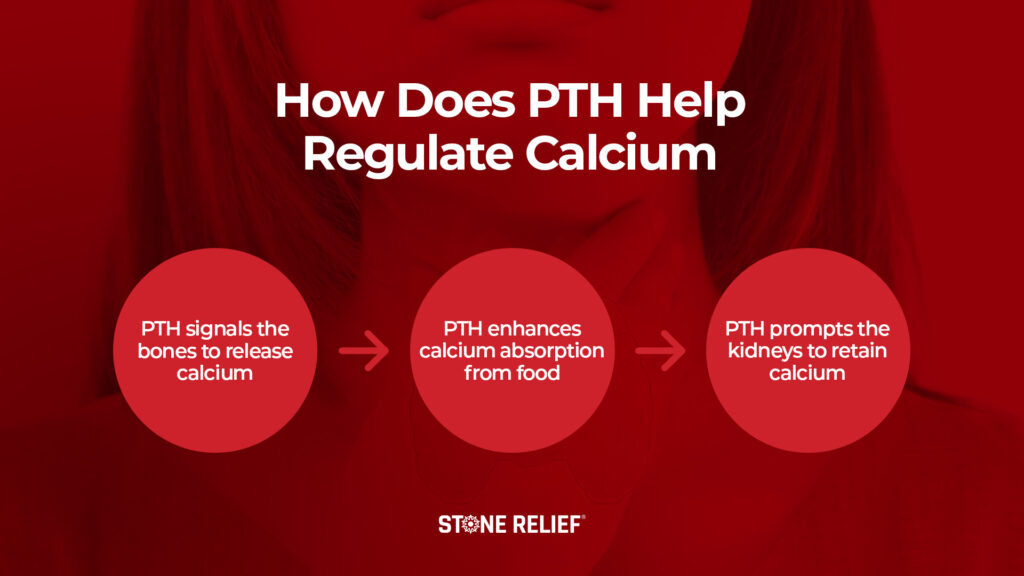
Again, the parathyroid glands make a hormone called PTH, which helps balance your body’s calcium levels. When calcium levels drop, they release PTH to bring them back up. The PTH helps boost calcium levels in three ways:
- Bone Resorption: PTH signals the bones to release calcium into the bloodstream. Back in elementary school, there was always a bully kid who loved pulling down his classmates’ pants. That’s how PTH strips calcium from your bones ????
- Intestinal Absorption: PTH signals the kidneys to produce more active vitamin D to enhance calcium absorption from the food you eat.
- Kidney Function: PTH prompts the kidneys to retain calcium rather than excrete it in urine. Think of it like a dam. When water levels are low due to less rainfall, operators will limit the water going through pipes to preserve the supply. This is the same concept happening in the kidneys. Normally, this causes low urinary calcium levels.
However, in hyperparathyroidism, too much PTH is produced, which causes high calcium levels in the blood and urine.
Hyperparathyroidism is classified into two types: primary and secondary.
Primary hyperparathyroidism directly affects the parathyroid glands. “Primary” means it starts in these glands, not because of another issue, like kidney problems. In this condition, one or more glands become too active and produces too much PTH.
In the US, around 100,000 people get primary hyperparathyroidism each year, making it one of the most common hormonal disorders. It’s more common in males than females, with a ratio of about 3-4 to 1, and often occurs in people aged 50 to 60.
Secondary hyperparathyroidism, though rare, happens due to other conditions like kidney failure or severe lack of vitamin D, causing an indirect effect on the glands. These conditions cause the parathyroid glands to grow bigger and produce more PTH.
Since excess PTH is directly linked to calcium regulation, let’s move on to the next section to better understand how this condition affects the risk of forming calcium-based kidney stones.
Hyperparathyroidism and Kidney Stone Connection
Around one-third of patients with primary hyperparathyroidism develop kidney stones. Most kidney stones are made of calcium oxalate, but slightly alkaline urine can also lead to calcium phosphate stones forming.
Let’s discuss why this condition can lead to these two stone types.
Calcium Oxalate Stones
Calcium oxalate stones (CaOx) mainly comprise calcium and oxalates. High urinary calcium levels would be insignificant without oxalates. According to studies, oxalates in plant foods are 15 to 20 times stronger in promoting this stone type than calcium. Let’s use a car as an example. Without fuel, a car won’t run. In the same way, without oxalates, even if your urinary calcium levels are high, no stones will form. It is safe to say that oxalates are the culprits for calcium oxalate stones.
But what about calcium phosphate stones? Is urinary calcium the enemy? Let’s find out in the next section.
Calcium Phosphate Stones
Calcium phosphate stones (CaP) require three things to form: high urinary calcium, high urinary phosphate, and alkaline urine (over 7.0 pH).
Aside from calcium, PTH also causes the bones to release more phosphate. This explains why people with hyperparathyroidism often have low phosphate levels despite absorbing more phosphate from food and having higher bone breakdown rates.
When urine is alkaline, calcium favors binding with phosphate instead of oxalates. Now, here’s the catch. Calcium and phosphate won’t cause stones without alkaline urine. In other words, alkaline urine is the major risk factor for calcium phosphate stones. It is like glue; calcium and phosphate won’t stick together without it.
So, don’t freak out if you produce excess PTH. It doesn’t mean you’ll automatically suffer from kidney stones. Oxalates and alkaline urine are the bad guys to keep out.
However, to add to your layer of protection, let’s talk about the causes of excess PTH so you will know what to troubleshoot.
Causes of Hyperparathyroidism
Hyperparathyroidism is highly connected to chronic calcium deficiency. The parathyroid glands are like a switch that turns on and off depending on blood calcium levels. For example, if blood calcium levels become low, the parathyroid glands will release more PTH. On the other hand, when you have enough calcium, PTH is not released. If you have been calcium deficient for a long time, it’s not impossible to develop this condition.
Also, vitamin D and vitamin A toxicity due to long-term intake of synthetic supplements can badly affect your parathyroid glands. The body doesn’t recognize synthetics. Synthetics also strain your liver and kidneys. When your kidney function is impaired, calcium regulation in the body is affected. This can cause hyperparathyroidism (secondary) over time.
Do you see the pattern? Hyperparathyroidism is highly related to DIET.
Nevertheless, there are also minor causes such as follows:
Heredity – Some rare hereditary conditions can impair the parathyroid glands.
- Multiple Endocrine Neoplasia Type 1 (MEN1) – A genetic disorder that causes tumors in the body’s glands, including the parathyroid glands, leading to overproduction of hormones.
- Multiple Endocrine Neoplasia Type 2A (MEN2A) – Another rare genetic disorder involving tumors, particularly the thyroid gland and parathyroid glands (located in the neck) and adrenal glands (located on top of the kidney).
- Familial Hyperparathyroidism – A hereditary condition where a person has an increased risk of developing overactive parathyroid glands.
- Hyperparathyroidism – Jaw Tumor Syndrome – A rare genetic disorder characterized by developing parathyroid tumors and tumors or cysts in the jawbone.
Milk-alkali syndrome – This condition develops due to long-term calcium supplementation.
Hyperplasia – The parathyroid gland enlarges due to constant stimulation of PTH. Around 15% of patients have hyperplasia.
Cancer – Around 1% to 4% of patients with hyperparathyroidism have parathyroid cancer.
Since we already know what causes hyperparathyroidism, let’s use this information to our advantage. The following section will teach you some strategies to treat/prevent excess PTH and lower kidney stone risk.
Treatment and Prevention Strategies
Dietary modification is the best way to treat/prevent hyperparathyroidism and kidney stones. That’s why we are inviting you to join our Coaching Program. This program will help you develop a personalized strategy to ensure your diet has enough vitamins and minerals to manage hyperparathyroidism and kidney stones. The goal is to maintain proper calcium, phosphorus, vitamin D, and vitamin A intake through REAL foods.
Speaking of REAL foods, we mean species-appropriate foods like meat, dairy, and seasonal ripe fruits. Avoid toxic plant foods because they are mostly high in oxalates and alkalize your urine!
Diet is more powerful than medications (e.g., Cinacalcet) and surgery (e.g., Parathyroidectomy) for hyperparathyroidism. Drugs and surgery don’t guarantee that your problems are solved. In fact, they are like patches on a torn garment. Eventually, the patches are no longer effective. The initial tear (condition) worsens.. You need a new garment – a new DIET to fix your hyperparathyroidism and kidney stone issues for good.
If you feel this is the best time to take on the RIGHT diet journey with us, check out our Coaching Program now!
REFERENCE:




Again a great blog. Thanks for sharing, ultimately the single source of truth for any kind of stone is dietary modification and mostly converting from a veg diet to a non veg diet. Am I correct ?
Hey @animesh , the degree to which the switch to a carnivore or animal-based diet will be determined by the type of stone you’re forming. But, as a baseline, if you eat this way, stones will no longer be an issue. The only real exception to this is cystine stones.
How does one test for hyperparathyroidis?
Hey @purplequeen , probably something to discuss with your general practitioner if you’re concerned. But, a simple blood test is where most start.